まなみ歯科へのリンク
Dental Caries: The Disease and Its Clinical Management
Part VI Caries control and prevention
P505
Chapter 28 Caries control for populations
28章 集団の齲蝕管理
V. Baelum, A. Sheiham and B. Burt
P505-26
Introduction
導入
The caries decline and changes in the practice of dentistry
齲蝕の減少と歯科診療の変化
Why does caries occurr?
なぜ齲蝕は生じるのか?
Upstream or downstream: does it matter?
上流か下流か: それが課題なのか?
Sick individuals or sick populations?
病んだ個人か、病んだ集団か?
Options for change: which preventive strategy should be used?
変化のための選択肢: どの予防戦略を選ぶべきなのか?
The high-risk approach
ハイリスクアプローチ
The population strategy for caries prevention
齲蝕予防のための集団戦略
The directed population strategy
標的集団戦略
A short history of caries-preventive strategies for populations
齲蝕予防の集団戦略小史
A wider perspective on prevention
予防の幅広い展望
Wanted: a population-based common risk factor approach to prevention
求む: 集団単位の予防の共通の危険因子手法
Where does this leave the traditional dentist? Need for a new professionalism
これは、どこで、従来の歯科医師を置き去りにするのか?新たなる専門性の必要性
References
P506
Introduction
導入
The disease processes leading to dental caries must undergo lifelong control (Griffin et al., 2005) in order to avoid the irreversible consequences of the later stages of caries development, namely cavity formation, restoration and the ensuing re-restorations, endodontic treatment, crown therapy, and possibly the ultimate loss of the tooth.
齲蝕の進行の最終段階、すなわち齲窩の形成、修復、再発による再修復、歯内治療、歯冠修復、そして一体どうしたものか、歯の喪失に至る不可逆的な帰結を避けるためには、歯の齲蝕に至る疾病の過程を、生涯にわたり管理しなければいけない (Griffin et al., 2005)。[歯のある限りにおいては...ね]
Therefore, the word ‘prevention’ is used to mean preventing the occurrence of the irreversible caries signs and symptoms by controlling the caries process.
すったもんだで‘予防’という言葉は、齲蝕の過程を管理することで、不可逆的な齲蝕の徴候と症状の発生を予防するという意味で使われている。
In this chapter, the authors argue the need to apply a common risk factor approach to prevention, for health promotion cannot be compartmentalized to specific parts of the body.
本章は、予防のための共通の危険因子手法を適応する必要がある、と主張する。というのも、健康づくりは全身の特定部分を切り離しては考えないからである。[common risk factorという表現はsocial determinantsへの挑戦が感じられないので、どうも、好きではないのですが]
Dental health is part of general health.
歯の健康は、全身の健康の一部である。
Any attempt to improve dental health should be fully integrated into broadly based health-promoting strategies and actions.
歯の健康を改善するあらゆる企ては、広範な支持基盤をもつ(多くの賛同を得た)健康づくり戦略と活動に、すっかり統合されるべきである。[2009.12.18]
It is thus worth keeping in mind that caries, periodontitis, oral mucosal lesions, oral cancer, temporomandibular joint dysfunction and pain are related to diet, tobacco, alcohol and stress; and that trauma to teeth is related to accidents.
齲蝕、歯周炎、口内粘膜病変、口内がん、顎関節の機能障害と疼痛は、食事、喫煙、アルコール、ストレスに、また、歯の外傷は事故に関連する、ということを忘れてはいけない。
Diet, alcohol, tobacco and stress are causes that are common to a number of chronic diseases such as cancer, heart diseases, diabetes and psychiatric diseases.
食事、アルコール、喫煙、ストレスは、がん、心臓疾病、糖尿病、精神疾病といった数多くの慢性疾病に共通している。
It is therefore rational to use a common risk factor approach (Sheiham & Watt, 2000; Griffin et al., 2005).
それゆえ、共通の危険因子手法を使う事は、合理的である (Sheiham & Watt, 2000; Griffin et al., 2005)。
This implies a new public health that is no longer oriented to single diseases, and preventive intervention approaches should no longer be organized around single clinical disease entities such as coronary heart disease, caries or cancer.
これは、もはや一つの疾病に指向するのではない新たなる公衆衛生を示唆しており、また予防介入手法はもはや、冠状動脈性心臓疾病、齲蝕、がんといった一つの臨床的疾病そのものに対して体系づけするのではない。[new public healthあるいはnew public health movementという言葉は、状況によって範囲に差異はあるようですが、おおむねオタワ憲章とその前後の脈絡における公衆衛生の方向性を指し示しているようです]
Most behavioral and social risk factors transcend these particular diseases, and instead influence susceptibility to diseases in general.
行動と社会の危険因子の大部分は、特定の疾病にとどまらず、むしろ全身の疾病の罹りやすさに影響している。
Moreover, decision makers and individuals will be more readily influenced by measures directed at the joint prevention of heart diseases, obesity, stroke, cancers, diabetes and dental caries than if disease-specific recommendations are made.
さらに、意思決定者と個人は、疾病特異的な勧告よりも心臓疾病、肥満、心臓発作、がん、糖尿病、齲蝕の合同予防を指向した方法に、影響されやすい。
Whenever possible, the strategies recommended for prevention and control of oral diseases, including dental caries, should therefore be part of a common risk factor approach to control the risks shared by a number of chronic diseases.
いつであれ、齲蝕を含む、口内疾病の予防と管理のために勧告される戦略は、多くの慢性疾病と共通の危険を管理するため、共通の危険因子手法の一部であるべきなのだ。[2009.12.19]
Such strategies involve food and health policies to change unhealthy dietary practices, a community approach to improve general hygiene (including oral hygiene), smoking cessation policies and policies on reducing accidents.
このような戦略は、不健康な食習慣を打開する食糧保健政策、(口内衛生も含んだ)衛生全般の改善への地域手法、禁煙政策、事故軽減政策からなる。[さりげなくstrategy=policyというすり替えが...]
These strategies should supplement the more disease-specific policies, which in the case of dental caries involve rational use of fluorides and the availability of appropriate, acceptable and evidence-based dental health care.
これらの戦略は、より疾病特異的な政策、齲蝕の場合は、フッ化物の合理的な利用、適切で受け入れやすく検証に基づいた歯科医療の入手可能性からなるが、その補足となるべきである。[suppement補足というより、mutually support相互支援とかそういう概念の方が適切だと思いますが...]
The caries decline and changes in the practice of dentistry
齲蝕の減少と歯科診療の変化
The past decades have witnessed a tremendous decline in the age-specific prevalence and extent of dental caries in many populations (see Chapter 8).
ここ数十年、齲蝕の年齢別有病数と有病割合の途方もない減少が、数多くの集団にて確認されてきている (Chapter 8を見ろ)。
This decline is well documented for child populations in the high-income countries (Helm & Helm, 1990; Downer, 1992; Marthaler et al., 1996; Davies et al., 1997) and to a lesser extent in adult populations (Truin et al., 1993; Marthaler et al., 1996; Kalsbeek et al., 1998; Eriksen, 1998).
この減少は、高所得国における小児人口 (Helm & Helm, 1990; Downer, 1992; Marthaler et al., 1996; Davies et al., 1997) に認められ、また成人にも若干の減少が認められる (Truin et al., 1993; Marthaler et al., 1996; Kalsbeek et al., 1998; Eriksen, 1998)。
Caries levels are also dropping in some high-caries populations, such as those in several Eastern European countries (Marthaler et al., 1996).
齲蝕水準は、東欧の国々の人々といった、一部の齲蝕多発集団においても低下している(Marthaler et al., 1996)。
Even though some believe that caries is generally increasing in Africa the available evidence suggests that the trend here is also downwards (Fejerskov et al., 1994; Cleaton-Jones & Fatti, 1999).
齲蝕はアフリカではおおむね増加していると思い込む人も、いるにはいるが、利用可能な資料によると、減少しているとのことである (Fejerskov et al., 1994; Cleaton-Jones & Fatti, 1999)。
This caries decline has been paralleled by important changes in the practice of dentistry.
この齲蝕の減少は、歯科診療における重大な変化と平行して生じている。
Where dental practice, as far as dental caries is concerned, only a few decades ago was almost entirely focussed on an operative treatment-oriented approach in the management of the most obvious cavities (Fejerskov & Kidd, 2003; Gimmestad et al., 2003; Hudson, 2004) and their sequelae, contemporary dental practice devotes more efforts to early (precavitation stage) caries diagnosis, and to non-operative and preventive care for such early lesions (Elderton & Eddie, 1983, 1986; Brennan et al., 1998; Brennan & Spencer, 2003a; Watt et al., 2004).
歯科診療は、齲蝕に関する限りでは、ほんの数十年前には、齲窩とその続発症の管理における手術指向手法に、ほぼ完全に焦点を絞っていた (Fejerskov & Kidd, 2003; Gimmestad et al., 2003; Hudson, 2004) が、現代の歯科診療はより早期(齲窩形成前)の齲蝕診断とそのような初期病変に対する非手術的予防的診療に力を注いでいる (Elderton & Eddie, 1983, 1986; Brennan et al., 1998; Brennan & Spencer, 2003a; Watt et al., 2004)。[標準的な歯科診療は、社会的個人的背景をもつ顎口腔系に対して包括的にアプローチするため、齲蝕に関する限りでは、という断り書きの意味するところは、よくわかりませんが...]
This trend for change seems particularly prominent in European dentistry, whereas US dentistry still tends to focus on restoring cavities (Ismail, 1997).
欧州の歯科においては顕著に、歯科診療に変化が生じているようであるが、合衆国の歯科学は、いまだに齲窩修復に焦点を絞っている傾向にある (Ismail, 1997)。
A key question is how this development should be interpreted.
鍵となる質問は、この改善はいかに解釈されるべきなのか、ということである。
Has the caries decline been brought about by a change of focus in dental practice away from its ‘drill, fill and bill’ perspective (Anusavice, 2005) to a more preventive attitude to the management of caries?
齲蝕の減少は歯科診療の焦点が‘形成、充填、請求’という考え方 (Anusavice, 2005) から、齲蝕の管理に対する予防的姿勢へ変化したことにより、もたらされたのであろうか?[んなわけねぇだろ、ってか]
Or does the increased emphasis on early diagnosis and preventive care merely reflect a response to the presence of steadily fewer overt cavities from a dental profession that wishes to keep a full appointment book, to maintain income and its raison d’être?
あるいは、早期診断と予防診療の強調は、着実に減少する齲窩を踏まえ、収入と存在理由を維持するために、約束帳をみつしりとさせたい歯科医師の思惑を、反映しただけだろうか?
Indeed, some studies suggest that the latter mechanisms also operate (Grembowski & Milgrom, 1988; Grytten, 1991; Grembowski et al., 1997; Brennan & Spencer, 2003b; Tickle et al., 2003b).
いかにも、いくつかの研究は、後者の機序がはたらいていることを示唆している (Grembowski & Milgrom, 1988; Grytten, 1991; Grembowski et al., 1997; Brennan & Spencer, 2003b; Tickle et al., 2003b)。
It is very tempting for members of the dental profession to try to take all the credit for the caries decline.
歯科医師団体の会員は、齲蝕の減少のすべての功績をかっさらおうと、必死である。
However, there are no reasons to do so, certainly as far as daily chairside preventive activities are concerned (Sheiham, 1997; Wang, 1998).
だが!齲蝕の減少に日々の臨床予防活動が関係しているという根拠は、ない (Sheiham, 1997; Wang, 1998)。
The chairside preventive armamentarium available to dentists is relatively limited, encompassing oral hygiene instructions (Davies et al., 2005), dietary advice (Lingstrom et al., 2003; Watt et al., 2003), pit and fissure sealants (Mejare et al., 2003; Locker et al., 2003; Ahovuo-Saloranta et al., 2004), and topical fluoride applications (Marinho et al., 2002a, b, 2003c, d; Hawkins et al., 2003; Seppa, 2004) given on an individual basis to people who for the most part appear in the dental office only once or twice a year.
歯科医師の利用できる臨床予防ツールは、至って限られており、大部分が、年に1回か2回の歯科診療室に訪れる人々に、個人単位で処置される、口内衛生指導 (Davies et al., 2005)、食習慣指導 (Lingstrom et al., 2003; Watt et al., 2003)、小窩裂溝填塞 (Mejare et al., 2003; Locker et al., 2003; Ahovuo-Saloranta et al., 2004)、フッ化物の局所応用 (Marinho et al., 2002a, b, 2003c, d; Hawkins et al., 2003; Seppa, 2004) からなる。
Even though the dentist may individualize the recall intervals and the contents and intensity of the preventive chairside sessions to reflect the actual caries situation for the person in question (see Chapter 14), there is very limited evidence to suggest that annual or biannual recalls, even when they include oral hygiene instructions (Beirne et al., 2005) (see Chapter 15) and individualized dietary counseling (Lingstrom et al., 2003) (see Chapter 19), will affect caries development or progression.
歯科医師は、患者本人の齲蝕状況を考慮し、リコール間隔と内容、臨床予防活動の度合いを個人にあわせている (Chapter 14を見よ) にもかかわらず、またその活動として、齲蝕の進行に影響を及ぼす口内衛生指導 (Beirne et al., 2005) (Chapter 15を見よ) と食習慣相談 (Lingstrom et al., 2003) (Chapter 19を見よ) を行った時でさえ、年1回あるいは2回のリコールを支持する資料はほとんどない。
There is some evidence from clinical efficacy trials that the professional application of topical fluoride in the form of gels, mouthrinses or varnishes results in only small caries reductions on top of those found from fluoride toothpaste alone (Marinho et al., 2004a).
フッ化物配合歯磨剤に加えて、歯科医師による、ジェル、洗口液、ワニスという局所フッ化物応用をすると、わずかな齲蝕の減少が認められる、という臨床効果試験の資料はある (Marinho et al., 2004a)。
Indeed, analyses based on data from more than 15 000 children failed to demonstrate the expected negative association between the frequency of professional topical fluoride applications and the number of interproximal restorations placed (Eklund et al., 2000).
実際のところ、1万5000人以上の児童の資料を分析したが、歯科医師による局所フッ化物応用の頻度と隣接面修復の数に、期待されるような負の相関は見いだされなかった (Eklund et al., 2000)。
In addition, studies have indicated that the preventive care actually provided by general dental practitioners is ineffective in high-risk children (Tickle et al., 2003b).
さらに、研究は、一般的な歯科医師により提供される予防診療は、ハイリスク児童には奏効しないことを示唆している (Tickle et al., 2003b)。
Studies report that practitioners tend to provide prevention to asymptomatic patients in routine maintenance schedules rather than to patients at higher risk of caries (Eklund et al., 2000; Brennan et al., 2000; Brennan & Spencer, 2003b), and continue to perform early restorative intervention (Domejean-Orliaguet et al., 2004).
研究によると、歯科医師は、齲蝕ハイリスクの患者ではなく、無症候性の患者に、定期的な予防診療を提供する傾向があり (Eklund et al., 2000; Brennan et al., 2000; Brennan & Spencer, 2003b)、早期修復介入を演じ続ける (Domejean-Orliaguet et al., 2004) とのことである。[2009.12.20]
This lends further support to the notion that the caries decline may not be attributable to the effects of the professional chairside preventive activities to the extent that dental professionals would like to believe.
これは、突き詰めると、齲蝕の減少は、歯科医師による臨床予防活動の影響に起因するものではない、という考えを支持するものである。
A study conducted in the Nordic countries has revealed considerable intercountry differences in the caries-preventive methods used by the dental professionals, while the caries prevalence and severity was similar (Kallestal et al., 1999).
北欧の国々で行われた研究は、歯科医師の提供する齲蝕予防方法は、国家によりかなりの違いがあること、そして齲蝕有病割合と重症度には違いがないことを、明らかにしている (Kallestal et al., 1999)。
Finally, ecological analyses indicate that social factors, rather than dental services, explain the major part of the geographical variation in caries experience (Nadanovsky & Sheiham, 1994), just as the contribution of dental services to the decline in dental caries is very much smaller than commonly thought (Nadanovsky & Sheiham, 1994, 1995).
最後に、生態学的分析は、歯科医療よりむしろ社会的因子が齲蝕経験の地理的ばらつきの大部分を説明しており (Nadanovsky & Sheiham, 1994)、また齲蝕減少への歯科医療の貢献は、通俗に考えられているより、ずっとずっと小さいということを示唆している (Nadanovsky & Sheiham, 1994, 1995)。
These analyses showed that dental services could explain only about 3% of the differences in the changes in caries levels among 12-year-olds across 18 countries.
これらの分析は、歯科医療は18の国における12歳児の齲蝕水準の変化のばらつきの3%を説明していることを示した。
Most of the differences in the caries level changes were explained by broad socioeconomic factors, whether fluoridated toothpastes were included or not (Nadanovsky & Sheiham, 1995).
齲蝕水準の変化には、ばらつきがあるが、そのほとんどが、フッ化物配合歯磨剤に関係なく、さまざまな社会経済的因子により説明された (Nadanovsky & Sheiham, 1995)。
P507
Why does caries occur?
なぜ齲蝕は生じるのか?
Historically, the professional view on caries causation has been limited to a model consisting of the tooth, the dental plaque bacteria and sugars.
歴史的に、齲蝕の原因の専門的視点は、歯と、歯のプラーク微生物、そして砂糖からなる模型に縛られている。
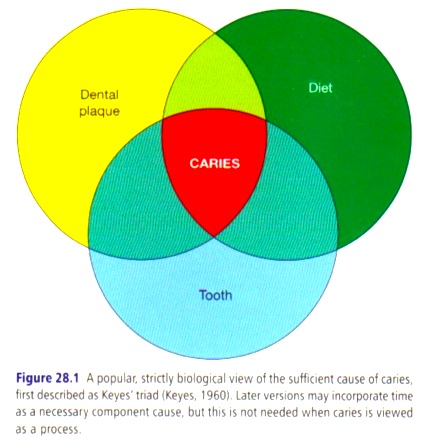 Together, these three necessary component causes form the biologically sufficient cause of caries, formerly known as Keyes’ triad (Keyes, 1960) (Fig. 28.1).
Together, these three necessary component causes form the biologically sufficient cause of caries, formerly known as Keyes’ triad (Keyes, 1960) (Fig. 28.1).
と同時に、これらの3つの必要構成要素は、齲蝕の生物学的に十分な原因を形作っており、これは以前には、keyesの三つの輪として知られていた (Keyes, 1960) (Fig. 28.1)。[2009.12.21]
From a theoretical standpoint, it is sufficient to block one of the component causes, e.g. the dental plaque bacteria or the intake of fermentable carbohydrates, to block the caries process.
理論上の見地からは、プラーク微生物か醗酵性炭水化物の摂取か、構成原因の一つを阻害すれば、齲蝕過程の阻害には十分である。
‘A clean tooth does not decay’ has been a mantra for many preventive activities over the years.
‘清潔な歯に、齲蝕は生じない’とは、長年多くの予防活動で唱えられているマントラである。
However, as the chairside caries-preventive activities, e.g. topical fluoride applications, oral hygiene instructions and dietary counseling, are specifically targeting each of these three necessary component causes, one may ask why these chairside preventive efforts have had such limited success.
局所フッ化物応用、口内衛生指導、食習慣相談といった臨床齲蝕予防活動は、これら3つの必要構成原因のいずれかを狙うのだが、これらの臨床予防活動はどうして成功しないのだろう、といぶかしむ[鈍い]人もいるだろうか。
P508
The answer is that dental researchers and clinicians alike have failed to grasp fully what caries causation is about.
その答えは、歯科研究者と臨床家が一様に、齲蝕の原因がなにであるかを、完全には把握していないことにある。
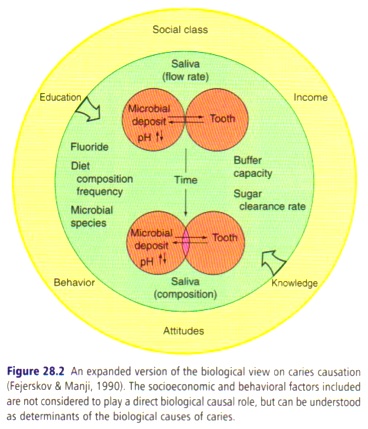
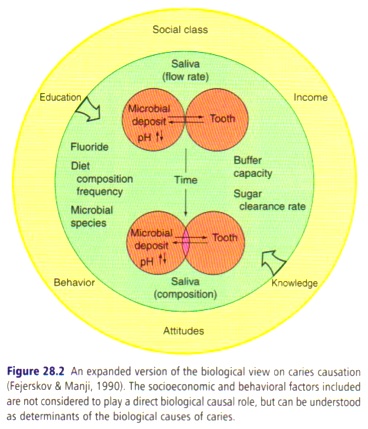 Even though more recent versions of the Keyes’ triad have expanded the strictly biological causal model by adding more distant causes (Fejerskov & Manji, 1990) (Fig. 28.2), and despite the terms ‘complex’ and ‘multifactorial’ now being quoted in almost any statement pertaining to caries etiology, most still erroneously misunderstand the etiology of caries by considering it as a purely biological process (Holst et al., 2001).
Even though more recent versions of the Keyes’ triad have expanded the strictly biological causal model by adding more distant causes (Fejerskov & Manji, 1990) (Fig. 28.2), and despite the terms ‘complex’ and ‘multifactorial’ now being quoted in almost any statement pertaining to caries etiology, most still erroneously misunderstand the etiology of caries by considering it as a purely biological process (Holst et al., 2001).
Keyesの三つの輪の最新版は、より遠い原因を加えた、生物学的に厳密な模型に拡張され (Fejerskov & Manji, 1990) (Fig. 28.2)、また、いまや齲蝕の病因論と抱き合わせの言い回しとなっている‘複雑’とか‘多因子’とかいう用語が横行しているものの、ほとんどの歯科医師は、それを純粋に生物学的過程と考えることで、齲蝕の原因論を誤解している (Holst et al., 2001)。
This means that when dentists think about the causes of caries, they do not think beyond dental plaque bacteria and the dietary carbohydrates and sugars.
これは、歯科医師が齲蝕の原因を考えるとき、プラーク微生物や食事性の炭水化物と砂糖の向こう側には興味がない、ということを意味している。
However, this viewpoint leads to self-delusion.
しかし、この観点は、自己欺瞞そのものである。
For one thing, it ignores the causes of the causes (Holst, 2005).
何しろ、その観点は、原因の原因をないがしろにしている (Holst, 2005)。[2009.12.21]
The biological model for caries causation does not provide answers to a number of pertinent questions, such as: why do some people eat highly ‘cariogenic’ diets while others don’t? and why do some people maintain good oral hygiene while others don’t?
齲蝕の原因の生物学的模型は、以下のようなもっともな疑問に答えをもたらさない。なぜ、ある人は‘齲蝕原性’食品を摂取し、ある人は摂取しないのか。なぜ、ある人は良好な口内衛生を維持し、あるひとは維持しないのか。
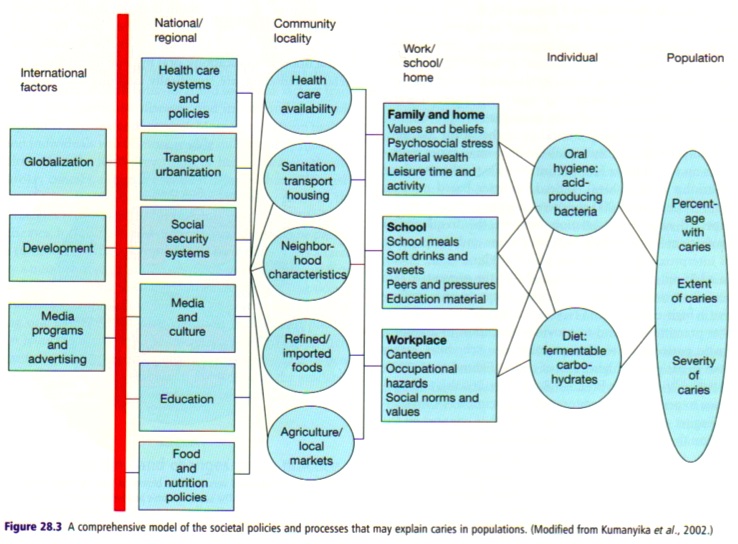
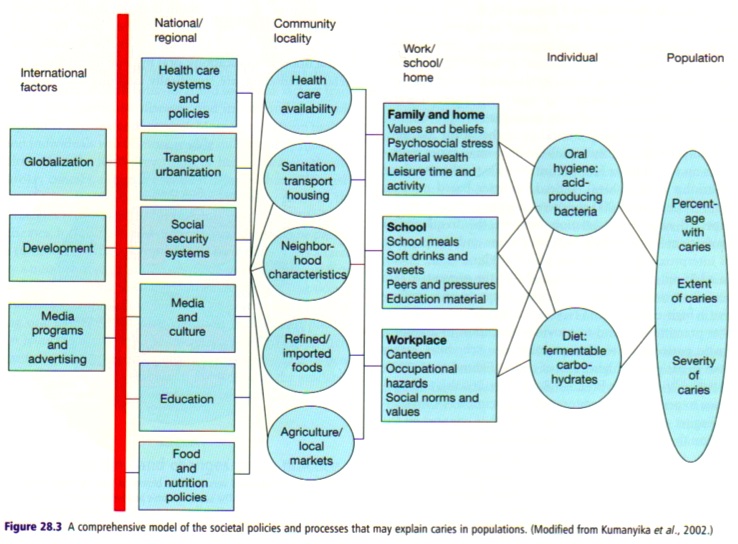 The second major limitation of the biological model for caries causation (Figs 28.1, 28.2) is that it understands causes as properties of individuals and ignores structural and contextual causes (Fig. 28.3).
The second major limitation of the biological model for caries causation (Figs 28.1, 28.2) is that it understands causes as properties of individuals and ignores structural and contextual causes (Fig. 28.3).
齲蝕の原因の生物学的模型 (Figs 28.1, 28.2) の第二の大きな限界は、個人の特性を原因として考え、構造的脈絡的原因を無視することにある (Fig. 28.3)。
Structural causes in relation to caries are those international, national, regional or local societal circumstances (e.g. industry, media, politics, economics, infrastructure) that affect the social context in which people live, e.g. the psychosocial environment, material wealth, workplace, home, and school (McMichael, 1995; Brunner & Marmot, 1999).
齲蝕に関連する構造的原因は、心理社会的環境、物質的豊かさ、職場、過程、学校といった、人々の生活する社会的脈絡に影響を及ぼす、国際的、国内的、地域的、局地的社会的環境(例えば、産業、メディア、政治、経済、社会基盤)からなる (McMichael, 1995; Brunner & Marmot, 1999)。[さりげなくMarmot登場]
The social context, in turn, shapes the behaviors, values and beliefs of individuals (Jarvis & Wardle, 1999; Chin et al., 2000).
社会的脈絡は、いわば、個人の行動、価値、信念を形作っている (Jarvis & Wardle, 1999; Chin et al., 2000)。
Based on these findings it is clear that if one wants to change people’s behaviors, a change is necessary in the environment that leads to the unwanted behaviors.
これらの知見を踏まえると、人々の行動を変化させたければ、望まぬ行動を導いている環境を変化させる必要があるのは、明らかである。
Dentists’ chairside preventive activities are largely based on a somewhat naive idea (Watt, 2002), the knowledge-attitude-behavior (KAB) model (Chin et al., 2000).
歯科医師の臨床予防活動は、概ね思いつき (Watt, 2002) や知識態度行動 (KAB) 模型に基づいている (Chin et al., 2000)。
According to the KAB model, individuals behave rationally and always make choices that serve their best interests.
KAB模型によれば、個人の行動は、常に合理的に得策を選択する (Chin et al., 2000)。
The idea is that knowledge provided to the individual (e.g. information about the unhealthy consequences of the current dietary and oral hygiene practices and advice/instructions for change) will bring about a change in the individual’s values and beliefs and attitudes which, in turn, will result in the desired behavioral change (e.g. improved oral hygiene practices or healthier dietary habits).
この考え方によると、個人は知識(現在の食事や口内衛生の成れの果てについての情報や変化の指導)によって価値観や信念、態度を変容する、つまり、(口内衛生や食習慣の改善といった)望ましい行動変容を引き起こす。
However, the available evidence generally suggests that the effects of such approaches, if at all demonstrable, are transient and of short duration (Kay & Locker, 1996; Watt & Marinho, 2005), and do not affect caries experience (Vanobbergen et al., 2004).
しかし、利用可能な資料によると、こういった手法の影響は、仮に変容が生じたとしても、一過性かつ短期間であり (Kay & Locker, 1996; Watt & Marinho, 2005)、齲蝕経験には影響しない (Vanobbergen et al., 2004)。[2009.12.22]
The basic problem is that the approach fails to understand that individual behaviors are also shaped by contextual and societal factors that cannot be reduced to individual attributes (Chin et al., 2000; Holst, 2005).
この手法の課題は、個人の行動は個人ではどうにもならない脈絡的社会的因子により形作られているということを理解し損ねていることにある (Chin et al., 2000; Holst, 2005)。
P509
There are numerous examples of the influences of such factors (Chin et al., 2000).
このような因子の影響の例は、ちょっと多い (Chin et al., 2000)。
 In a dental context (Fig. 28.4), there are good reasons why the sweet shelves in the supermarkets are invariably placed near the checkout counter, where shoppers and their impatient children have to stand in line.
In a dental context (Fig. 28.4), there are good reasons why the sweet shelves in the supermarkets are invariably placed near the checkout counter, where shoppers and their impatient children have to stand in line.
歯科と関連ある事例 (Fig. 28.4) で挙げると、スーパーマーケットの御菓子棚は、いつも、買い物客とせっかちな小児が列を作るレジのそばにあるが、これには、ちゃんとした理由がある。[2009.12.23]
There are also good reasons why soft-drink companies have entered into contracts with school districts in the USA that give the companies exclusive rights to stock their products in the schools’ vending machines (Heller et al., 2001).
清涼飲料水企業は、合衆国の通学区域と、学校の自動販売機に自社商品の仕入れの独占権契約を結ぶ (Heller et al., 2001) が、これにも、ちゃんとした理由がある。
There are good reasons why a person, who lives in a social context where the tradition for oral hygiene procedures is limited and where toothache and tooth loss due to caries are seen as inevitable consequences of life, does not respond positively with the desired behavioral change when dental professionals give advice about the likely benefits of tooth brushing twice a day using fluoride toothpaste.
口内衛生手段の習慣がない社会脈絡のなかで生活する人や、齲蝕による歯痛と歯の喪失が人生の必然である地域に生活する人が、歯科医師が一日二回のフッ化物配合歯磨剤を利用した歯磨きのすぐれた恩恵について助言を受けても、望ましい行動変容に積極的に反応しないのにも、やはり、ちゃんとした理由がある。
Similarly, a person cannot be expected to stop smoking when everyone they live with, work with and spend their leisure time with smokes.
同様に、喫煙をする家族や同僚、友人がいれば、一人で禁煙をできるという道理はない。
Countless smokers will testify to the fact that the ‘advice’ typically given by the resourceful, to pull oneself together, rarely suffices to achieve permanent smoking cessation.
数えきれない喫煙者が、自制心をとりもどせ、という典型的な‘助言’は、永続的な禁煙には、正直役に立たないと証言するだろう。
It is not a trivial matter of providing more knowledge about caries and obesity, for a person used to frequent snacking, to cause him or her to abandon this habit when such snacking behavior is the norm in her social context, e.g. the family, workplace, or school.
間食が、家族や職場、学校といった社会的脈絡における規範である場合、よく間食をする人物がこの習慣を捨て去るには、齲蝕と肥満についてのさらなる知識を提供すればいい、というものではない。[2009.12.24]
Similarly, it is much more difficult to convince young people that regular intake of large quantities of sugar-containing carbonated soft drinks is a bad idea from a caries and obesity perspective when multinational companies are allowed to use the youth culture media to portray this behavior as synonymous with success.
同様に、多国籍企業が、ラージサイズの砂糖添加炭酸清涼飲料水を日常的に摂取することを成功の代名詞として若者文化のメディアに浸透させている場合、若年者を、齲蝕と肥満の観点から、それはよからぬことである、と説得するのは困難である。
P510
These arguments all point in one direction: if dental professionals really mean to bring about reductions in caries levels in the populations they serve, they need to comprehend the causes of caries beyond the strictly biological (Holst et al., 2001; Newton & Bower, 2005; Holst, 2005).
これらの論争には、一つの方向がある。もし歯科医師が集団の齲蝕水準の低下を引き起こすつもりであれば、齲蝕の原因を、厳密な生物学を越えて、よく理解する必要があるということだ (Holst et al., 2001; Newton & Bower, 2005; Holst, 2005)。
Upstream or downstream: does it matter?
上流か下流か: それが課題なのか?
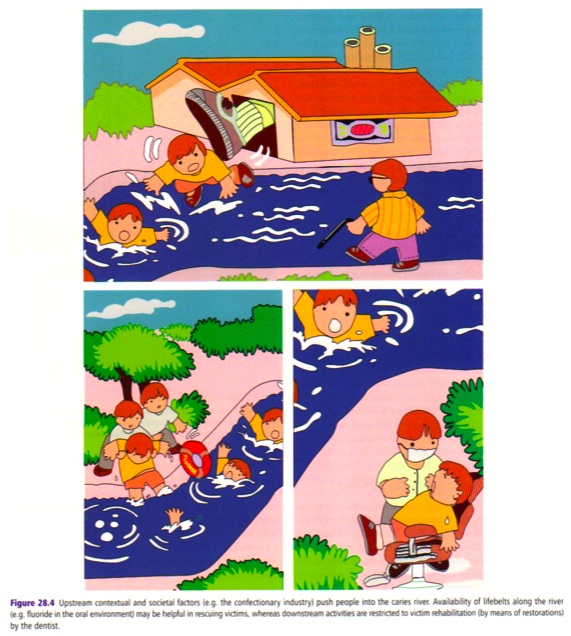
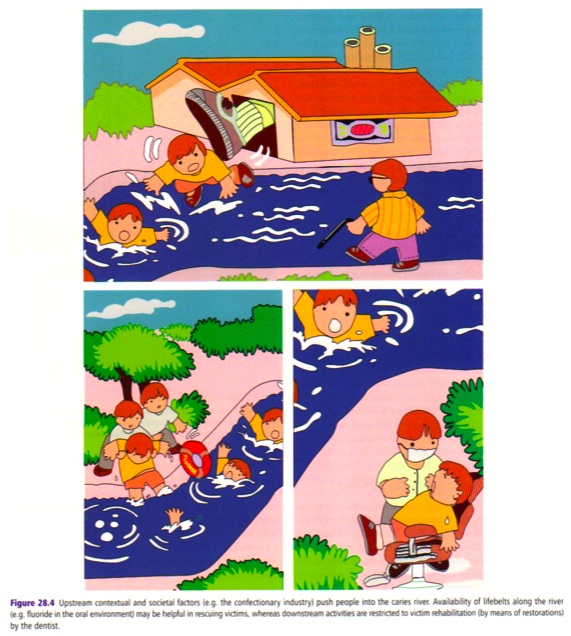
The failure of the present dominant dental approach to the prevention of caries in populations can be illustrated by an allegory.
現在支配的である、集団の齲蝕予防の歯科手法の不成功は、寓話により示される。[この寓話のオリジナルは(McKinlay 1979)]
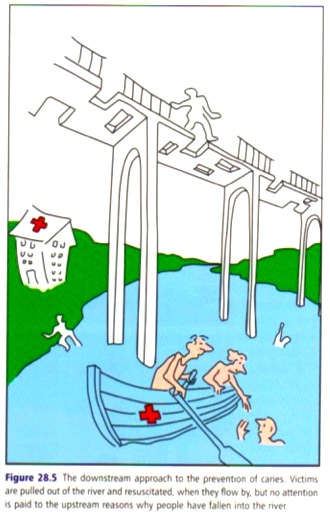 A doctor was standing by the side of a river and heard the cry of a drowning person, who had fallen off the bridge crossing the river (Fig. 28.5).
A doctor was standing by the side of a river and heard the cry of a drowning person, who had fallen off the bridge crossing the river (Fig. 28.5).
医師は川のそばに立っており、川を渡る橋から落下して流される人の叫び声を聞いているのだ (Fig. 28.5)。
He jumped in to rescue and to resuscitate him.
医師は、彼を救出、蘇生するために川に飛び込む。
Just as the rescued man was recovering on the river bank there were more cries from other drowning people.
救出者が土手で回復するや否や、流された人々のさらなる叫び声が聞こえてくる。
The rescuer jumped in again, brought some back and resuscitated them.
救助者はふたたび川に飛び込み、これらを蘇生する。
The rescuer could not cope alone, so he fetched helpers and breathing machines.
救助者は一人ではどうにもならず、助けをよび呼吸器をそろえる。[地方に医師と予算が足りない!ってやつですな]
Still he could not cope.
それでも救助者は、うまく対処できない。
So they worked faster in teams, four-handed and six-handed, with more complex equipment and faster methods of resuscitation.
そのため、救助者は二人組みで、そして四人組みで団結し、より複雑な装備とより迅速な蘇生方法にて、高速救助に取り組む。
So many people were drowning that some could not be rescued before permanent damage had occurred.
あまりに多くの人々が流されてくるため、救出に間に合わず、永久的な損傷が生じてしまう。
How could he stop them from drowning?
どのように、彼らが溺れるのを止められるだろうか?
Swimming lessons were his solution.
水泳訓練が解決を導くだろう。
Health education.
健康教育が解決を導くだろう。
However, rescuing and swimming lesson activities kept the available doctors so busy that at no time did they stop to consider why people who could not swim were in the river in the first place.
しかし、救助と水泳訓練活動は、活動可能な医師をがっしりと縛り付けるため、立ち止まって、まず第一に、なぜ泳げない人々が川にいるのか、を考えようとする医師は、いない。
Who was pushing them in upstream (Pearce, 1996; Watt, 2007)?
だれが、医師を上流へ後押しするというのか (Pearce, 1996; Watt, 2007)?[2009.12.25]
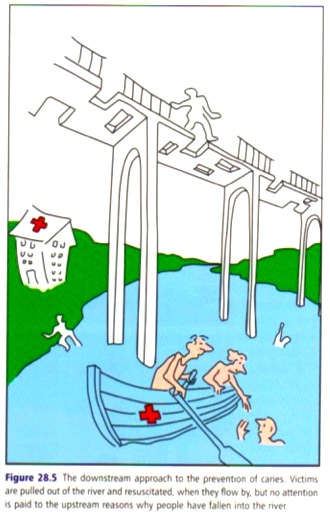
 Had the doctors had time to contemplate they would soon have realized by mere inspection of the bridge that simply providing the bridge with proper railings would have prevented many people from falling off the bridge (Fig. 28.6).
Had the doctors had time to contemplate they would soon have realized by mere inspection of the bridge that simply providing the bridge with proper railings would have prevented many people from falling off the bridge (Fig. 28.6).
もし医師に、沈思する時間があったのなら、橋を調査して、橋に適切な手すりをつけるだけで多くの人々が橋から落下するのが防がれることを認識していたであろう (Fig. 28.6)。
Stopping people from falling off the bridge or making the river shallower, by health promotion, will prevent people from drowning even if they cannot swim.
たとえ人々が泳げなかったとしても、健康づくりにより、人々が橋から落ちるのを止めることや川を浅くすることで、人々が溺死するのを防げる。
The dentists’ concentration on the downstream victim rescue operation had completely distracted their attention from the upstream activities of the confectionery, food and drink companies who were ‘pushing people into the water’ (Fig. 28.4); just as it prevented dentists and their professional bodies from lobbying and putting pressure on politicians and other decision makers that unhealthy choices could be made more difficult (and healthy choices easier) if appropriate regulations were instigated.
歯科医師の下流の犠牲者救出作戦への集中は、おかし、食品、飲料企業が上流で行っている‘川に向かって人々の背中を押す’活動から、見事に注意をそらし (Fig. 28.4)、歯科医師や専門機関が、政治家やその他の意思決定者に、適切な条例が成立すれば不健康な選択をより困難にする(と同時に、健康的な選択が易しくなる)ということを、陳情するのを妨ぐ。[2009.12.26]
What this allegory suggests is that more efforts should be directed at making healthy choices the easier choices, and at controlling the activities of those pushing people into the water, i.e. a direct attack on the determinants of health.
この寓話は、健康的な選択をより易しい選択にすることに、そして人々を川へ後押しする活動の管理、すなわち健康の決定要因への取り組みに、より多くの努力を払うべきであるということを示唆している。[making the healthier choices the easier choiceのオリジナルはNancy Milio (1986)]
While dentists need not completely abandon their down-stream activities in the form of evidence-based oral hygiene instructions, dietary counseling and topical fluoride applications, they should be aware of their limitations and realize that midstream activities, such as supportive health promotion, and upstream activities, such as appropriate regulations aiming at making healthier choices easier and unhealthy ones more difficult, carry much larger benefits for the population’s health (Fig. 28.4).
歯科医師は検証に基づいた口内衛生指導、食習慣相談、局所フッ化物応用といった下流の活動を完全に中止する必要はないが、それらの限界とともに、健康づくりの支援といった中流活動、健康的な選択を易しい選択にし、不健康な選択を困難な選択とする条例の議決といった上流活動は、集団の健康により大きな恩恵をもたらす、ということを認識すべきだろう (Fig. 28.4)。
P511
Sick individuals or sick populations?
病んだ個人か、病んだ集団か?
It is the centerpiece of appropriate clinical dentistry to ask not only ‘what is the diagnosis, and which is the best treatment for this tooth?’, but also ‘why did this occur, and could it have been prevented?’ (Rose, 1985).
‘診断は何か、そしてこの歯に対する最善の治療はどれか?’という問いと‘なぜこれが生じたのか、そしてこれは防げたのか?’という問いは、適切な臨床歯科の目玉的存在である (Rose, 1985)。
These questions arise out of the clinical dentists’ natural concern for the patient, the sick individual.
これらの疑問は、臨床歯科医師の、患者や病んだ個人に対する自然な気遣いから、生じる。
However, restricting oneself to this perspective is tantamount to not being able to see the forest for the trees.
しかし、この観点に自己を制限することは、木を見て森を見ないことと同じである。
The dental profession is also obliged to ask the question why some populations or groups have severe caries while in others caries is considerably less extensive.
歯科医師には、なぜ、ある集団の齲蝕は重度であり、その他の集団の齲蝕は見違えるほど軽度であるのか、という疑問に答える義務もある。
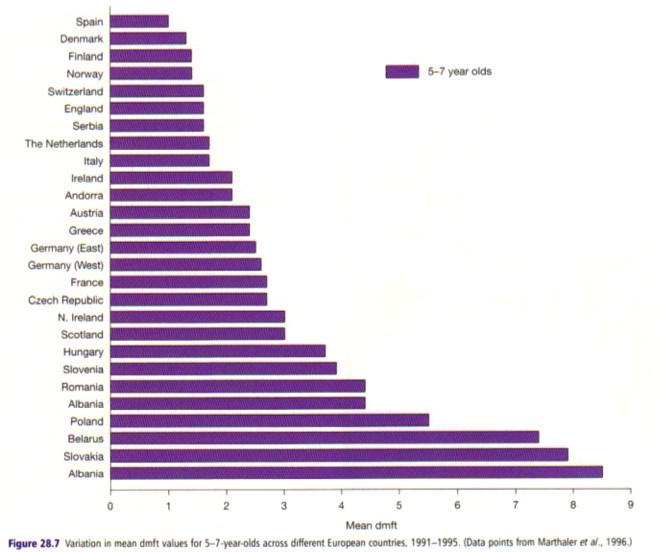
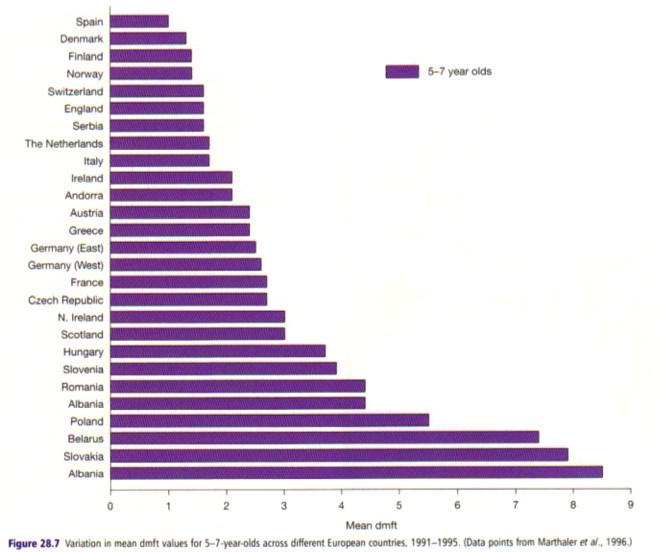 Figure 28.7 is just one of many possible illustrations that demonstrate the huge variation in the extent of caries recorded at the cavitation level across different populations.
Figure 28.7 is just one of many possible illustrations that demonstrate the huge variation in the extent of caries recorded at the cavitation level across different populations.
Figure 28.7は、さまざまな集団における齲蝕水準には、大きなばらつきがあるということを示している可能性がある。
There was an eight-fold difference in the average number of decayed, missing, or filled primary teeth (dmft) among 5-7-year-old children between the most extensively affected European population (Albania; dmft5-7=8.5) and the least affected population (Spain; dmft5-7=1.0).
5-6歳児の乳歯の齲蝕経験本数 (dmft) の平均を比較すると、欧州で最も齲蝕の吹き荒れているアルベニア (dmft5-7=8.5) と最も穏やかなスペイン (dmft5-7=1.0) の間には、8倍の襞がある。
Considerable variation is also present for population groups within nations.
国内の集団においても、大きなばらつきが存在している。
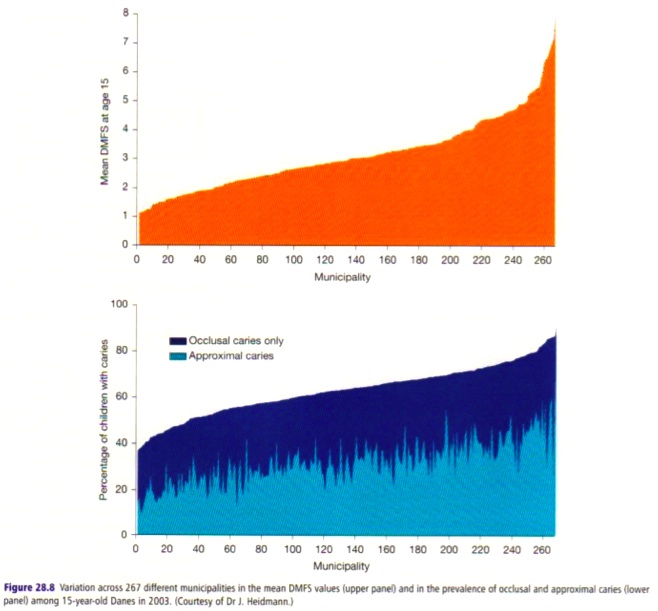
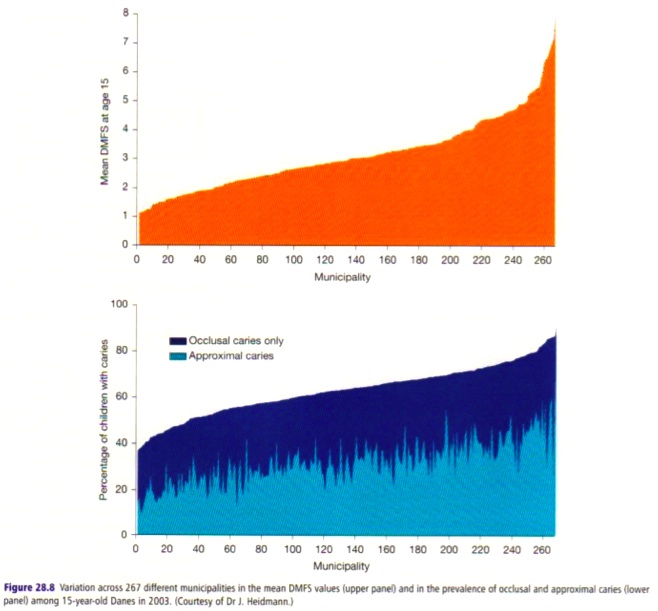 Even though Denmark, according to Fig. 28.7, has lower caries levels than most countries (in this case dmft among 5-7-year-olds), there is considerable intra-country variation between the different Danish municipalities (Fig. 28.8).
Even though Denmark, according to Fig. 28.7, has lower caries levels than most countries (in this case dmft among 5-7-year-olds), there is considerable intra-country variation between the different Danish municipalities (Fig. 28.8).
Fig. 28.7によれば、(5-7歳児DMFT指数では)ほとんどの国々よりも低い齲蝕水準であるデンマークであるが、地方自治体により大きなばらつきが存在している (Fig. 28.8)。
Within Denmark there is also an eight-fold difference in the average number of decayed, missing or filled permanent surfaces (DMFS) and a six-fold difference in the prevalence of caries at 15 years of age between the ‘best’ and the ‘worst’ Danish municipalities (Ekstrand et al., 2003).
デンマークの地方自治体の‘ベスト’と‘ワースト’は、15歳児のDMFS指数で8倍、齲蝕有病割合で6倍の襞がある (Ekstrand et al., 2003)。
Figures 28.7 and 28.8 show caries data on an aggregate level; namely as mean dmf/DMF scores for populations or groups within populations.
Figures 28.7と28.8は、集団内の一部におけるdmf/DMF指数の資料である。[2009.12.27]
These statistics do not usually attract much attention from clinical dentists, whose main concern is caries in the individual patient.
これらの統計は、一般的には臨床歯科医師の注意を引きつけない。彼らの主な関心は、患者個人の齲蝕なのである。
However, dentists are well aware that the caries experience of individuals may vary considerably among otherwise apparently similar individuals.
だが待ってほしい。歯科医師は、個人の齲蝕経験が、その他の点では一見よく似た個人であっても、大きく異なることを、知っているではないか?
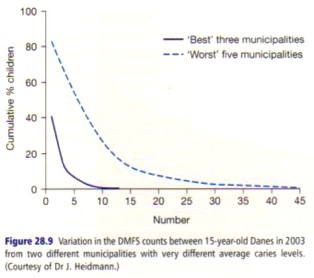
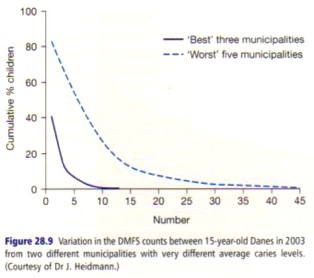 An example of such within-group variation of dental caries is seen in Fig. 28.9, which contrasts the caries experience recorded at the cavitation level of 15-year-old Danish children from ‘low’ and ‘high’ caries municipalities.
An example of such within-group variation of dental caries is seen in Fig. 28.9, which contrasts the caries experience recorded at the cavitation level of 15-year-old Danish children from ‘low’ and ‘high’ caries municipalities.
このような齲蝕の集団内のばらつきの一例を、Fig. 28.9に示す。ここでは、デンマークの15歳児の齲蝕の‘少ない’地方自治体と‘多い’地方自治体の記録と、対比している。
The distribution of DMFS is right-skewed in both the low and high caries groups, and the caries experience varies between children within each group.
DMFS指数の分布は、齲蝕の少ない集団と多い集団の両方で右に傾斜分布しており、齲蝕経験は、それぞれの集団内でばらつきがある。[2009.12.29]
However, in the low caries municipalities about 60% of the 15-year-olds are caries free (40% have caries), compared with 17% of the children in the high caries municipalities (where 83% have caries).
だが、もう一度待ってほしい。齲蝕の少ない地方自治体の15歳児の約60%は、齲蝕なし(40%は齲蝕あり)であるのに対して、齲蝕の多い地方自治体では17%が齲蝕なし(83%が齲蝕あり)なのだ。
More than 25% of the 15-year-olds in the high caries municipalities had at least 10 DMFS, while only 0.5% of the children in the low caries municipalities had a DMFS of 10 or more.
齲蝕の多い地方自治体の15歳児の25%以上は、最低でも10 DMFSであるが、齲蝕の少ない地方自治体で10 DMFS以上となるのは、小児では、0.5%のみである。
It is quite understandable that the response of the dentists when faced with such distributions is to concentrate on the characteristics of the children who suffer extensive caries, i.e. those in the right-hand tail of the distributions.
このような分布に直面した歯科医師の反応は、齲蝕の多い小児、すなわち分布の右側の裾野の特性に集中するということは、完全に理解可能である。
Hence, the answer to the clinical question ― why do some patients get extensive caries while other patients who live in apparently similar social circumstances are caries free or suffer only the occasional lesion? ― is based on an evaluation of differences in the characteristics of individuals and their families within the group.
それゆえ、臨床的な疑問―一見似たような社会的環境に生活する患者であるが、齲蝕なしでや咬合面齲蝕にとどまる患者がいる一方で、なぜ一部の患者に齲蝕が多発するのか
―への回答は集団内の個人と家族の特性の違いの評価に至る。
However, the answer to the question why some municipalities or countries suffer extensive caries, while others have little, has to do with the determinants of the population mean (Rose, 1985).
そこで、今一度待ってほしい。なぜ、齲蝕のほとんどない地方自治体や国がある一方で、一部の地方自治体や国には齲蝕が多発しているのかという疑問に、母平均の決定要因の観点から、回答すべきである (Rose, 1985)。
Unfortunately, these determinants are seldom of concern to the clinical dentist, because they are not found in the characteristics of the individual patients.
不幸なことに、これらの決定要因は、臨床歯科医師の注意をほとんど引いていない。それは、集団の健康の決定要因は、患者個人の特性からは見いだせないからである。
Instead, they are to be found in factors that produce a shift in the whole distribution of caries.
決定要因は、むしろ、齲蝕の分布の変化を生み出す因子から見いだされる。
Several studies have shown that the distribution of caries in a population can be predicted by the mean DMFS or DMFT scores (Jarvinen, 1985; Batchelor & Sheiham, 2002).
数多くの研究は、集団における齲蝕の分布はDMFS指数あるいはDMFT指数から予測されることを示している (Jarvinen, 1985; Batchelor & Sheiham, 2002)。
These results demonstrate that combating caries requires mass influences that act on the population as a whole; in other words, shifting the whole population’s mean to the left.
これらの結果は、齲蝕との戦いは、集団全体に大きな影響をもたらす必要がある、ということを示している。言い換えれば、母平均を左へ移動する必要があるということである。
P512
The above illustrates a very important point that is not well understood: the causes of individual cases of caries are not always the same as the causes of the incidence of caries, in populations (Holst, 2005).
上述は、あまりよく理解されていない、重要なポイントを示している。個人の齲蝕の原因と集団における齲蝕発生率の原因は、微妙に異なるのだ (Holst, 2005)。
The point is valid not only for caries but applies to essentially all diseases afflicting humankind (Rose, 1985, 1992).
このポイントは、齲蝕に有効なのはもちろん、人間を苦しめるすべての疾病に適応される (Rose, 1985, 1992)。
Options for change: which preventive strategy should be used?
変化のための選択肢: どの予防戦略を選ぶべきなのか?
So far, two fundamentally different approaches to prevention have been alluded to: the high-risk strategy and the population strategy.
ここまで、2つの予防のための手法をほのめかしてきた。すなわち、ハイリスク戦略と集団戦略である。
A third approach is used, namely the directed population strategy, also called geographic targeting, which is an amalgamation of the high-risk and the population strategies for prevention (Sheiham & Joffe, 1991).
また、第三の手法として、標的集団戦略、あるいは地理的標的戦略がある (Sheiham & Joffe, 1991)。これは、予防のためのハイリスクアプローチと集団戦略を組み合わせたものである。
It was the British epidemiologist Geoffrey Rose (Rose, 1992) who first defined the strengths and weaknesses of the high-risk and population approaches to prevention of chronic diseases, including caries.
イギリスの疫学者Geoffrey Rose (Rose, 1992) は、齲蝕など慢性疾病を予防するためのハイリスク手法と集団手法について、その利点と欠点を定義した、最初の人類であった。
P513
The high-risk approach
ハイリスクアプローチ
The high-risk approach to prevention is based on the concept that preventive efforts should be concentrated on that segment of the population that appears to have a high risk of disease.
予防のためのハイリスクアプローチは、予防努力は、疾病のリスクの高い一部の集団に集中すべき、という概念に基づいている。
For dental caries this corresponds to a concentration of effort on those individuals who are at a high risk of ending up in the right-hand tail of the distribution of caries experience (Fig. 28.9), while little attention is paid to the majority of the population with small or negligible individual disease risks.
これは、齲蝕の場合、齲蝕経験の分布 (Fig. 28.9) の右の端であるハイリスクの個人に努力を集中させることに対応しており、齲蝕のリスクが小さい、あるいはごく小さな集団の大部分には注意を払わない。
To be able to target this right-hand tail it is necessary to be able to predict future caries development.
この右端を標的にするためには、将来の齲蝕進行を予測する必要がある。
This topic is discussed in Chapter 29, which concludes that such prediction may be impossible.
このトピックスについてはChapter 29で触れているが、結論としては、齲蝕経験の予測は、できそうにない。
Even so, proponents of the high-risk strategy advocate this strategy on the basis of five principal arguments (Table 28.1).
とはいえ、ハイリスク戦略の推奨者は、5つの原則に基づいて、この戦略を推奨している (Table 28.1)。
・Intervention is appropriate to the individual: it makes sense to both dental professionals and patients at high risk and enhances motivation of both when dietary advice and oral hygiene instruction is given in response to unhealthy eating habits and poor oral hygiene conditions.
・介入は個人に適している: ハイリスク手法は、歯科医師とハイリスクな患者の互いに、つじつまがあっており、また、不健康な食習慣と劣悪な口内衛生状況に対して、食習慣の助言と口内衛生指導を行う際に、両者の動機を刺激する。
・No intervention with those not at special risk: if high risk of (extensive and severe) caries is confined to a minority, most people need not be troubled with preventive interventions as they have small risks.
・特別なリスクのない人々には介入しない: もし(重度の)齲蝕のハイリスクが少数に限定されれば、ほとんどの人々は、リスクのある予防介入に巻き込まれる不安がない。
Urging preventive actions on the caries free who are unlikely to benefit makes little sense, and may actually constitute bad advice if it involves costs or other risks.
恩恵の生じない、齲蝕のない人々に予防活動を要請することは、意味がほとんどない。そしてもし予防活動に費用やリスクがともなうのであれば、実際には役に立たな
い助言となりうる。
・Fits the ethos and organization of health-care systems: in dentistry, the link between curative and preventive actions has long been established.
・医療制度の風潮や組織に合致: 歯科では、治療と予防活動の連鎖が確立されて久しい。
Decades ago people went to the dentist mainly in response to subjective complaints, e.g. toothache.
数十年前、人々は主に主観的な不満、例えば歯痛のために歯科へ通っていた。
Today, dental attendance patterns are largely preventive: people who do not have symptoms go to the dentist for check-ups because this is considered good preventive behavior, a notion which most dentists fully advocate.
今日、歯科受診行動は、主に予防を目的としている。症状のない人々が歯科健康診断のため、歯科に行くのだ。なぜなら、それが、ほとんどの歯科医師が全面的に推奨する、よい予防行動であると考えられているからである。
・Cost-effective use of resources: resources for dental care are limited and some rationing is necessary.
・資源の費用効果的な利用: 歯科医療の資源は限られており、なんらかの配給が必要である。
Priority should be given to those who are likely to benefit (the most) from the intervention.
優先順位は、介入による恩恵の見込める集団に付けられるべきである。
・Improved benefit-risk ratio: if the risks of intervention are the same for everybody it follows that the benefit-risk ratio will be more favorable where the benefits are larger.
・損益比の改善: もし介入のリスクがだれでも同じであれば、ハイリスク手法は、恩恵を大きく、損益比をより良好にする。
However, the high-risk strategy for prevention has important disadvantages:
しかし、予防のためのハイリスク戦略には、より重大な欠点がある。[2009.12.30]
・Medicalization of prevention: Rose explains this problem using an anecdote about a man who went to see his doctor because of a pain in his neck, but walked away from the doctor’s office carrying the label ‘hypertensive patient’ and a prescription for antihypertensive drugs to be taken for the rest of his life (along with regular ‘preventive’ visits to the doctor).
・予防の医療化: Roseは、首痛のため受診するが、医師からは‘高血圧患者’と判断され、残りの一生において(‘予防’診察と抱き合わせで)降圧薬を処方される奇談を使い、この課題を説明している。
He went feeling ‘normal’ and left as a ‘patient’.
彼は‘健全’なつもりで受診したが、帰るときは‘患者’となっていた。
Hypertension is no more a disease than is dental plaque bacteria or bad dietary habits, yet this ‘labeling’ of a person as a patient will inevitably force him to think and act as a patient.
高血圧はプラーク微生物や乱れた食習慣がそうではないように、疾病ではないが、このように人を患者として‘レッテル貼り’することは、その人が患者として自認し行動することを避けようもなく強制する。
This may result in anxiety, impaired self-confidence or altered self-image in normal people.
これは不安と自信消失をもたらし、普通の人であるという自己像をぶっこわす。
Most practitioners will have met dental patients who are so downhearted by repetitive attempts to improve their oral hygiene that they actually ask us not to mention the problem anymore.
臨床医であれば、実際にはこちらが何も言っていないのに、口内衛生の改善を繰り返し試みて、落胆した歯科患者に遭遇するだろう。
・Palliative and temporary success: the high-risk strategy is about protecting against the effects of exposure (as might be achieved by frequent topical fluoride applications), or about lowering the exposure (e.g. by improved oral hygiene or altered dietary practices) among the high-risk individuals.
・姑息的一時的成功: ハイリスク戦略は、(局所フッ化物応用などにより)ハイリスク者を暴露の影響から保護するか、(口内衛生や食習慣の改善により)ハイリスク者への暴露を軽減する。
Neither of these two approaches deals with the basic reasons why people are exposed to the harmful determinants of caries.
これらの2つの手法は、人々がなぜ齲蝕の有害な決定要因に暴露されるのかという、根本的な原因を扱わない。
Their effects will therefore remain local, palliative and temporary.
そのため、これらの影響は、局所的姑息的一時的なものににとどまる。
Here are some analogies: ‘icebergs cannot be prevented by cutting off their tips, just as feeding the hungry does not tackle the causes of famine’.
ここには、ある一致点がある。‘氷山は一角を崩しても、防がれない。飢えた人々に食糧を与えても、飢餓に取り組んでいるとは言えない。’
・Behaviorally inadequate: along with most other lifestyle characteristics, people’s oral hygiene practices and dietary habits are shaped and constrained by the norms prevailing in their surroundings, whether in society at large or in their homes and families.
・行動的に不適切: その他の生活様式の特性とともに、人々の口内衛生と食習慣は、社会であろうと家庭や家であろうと、その環境で広く行き渡った規範により形作られ、強いられている。
Trying to behave differently from one’s family and friends is not an easy task, yet this stepping out of line is precisely what the high-risk approach to prevention is asking people with many problems to do.
家族や友人とは違った行動しようとすることは、易しいことではない。予防のためのハイリスク手法は課題のある人々にしてもらおうとしていることというのは、まさに、この社会通念からはずれる行動をしてもらおう、ということに他ならない。
・Poor prediction: application of the high-risk strategy to caries prevention necessitates identification of people at high risk of future caries development.
・予測が困難: 齲蝕予防のためのハイリスク戦略の応用には、将来の齲蝕進行のリスクの高い人々の同定が必要である。
As thoroughly discussed in Chapter 29, this may be a mission impossible.
29章で徹底的に論じることになるが、これは、困難を極める。
・Feasibility and cost problems: the costs of screening for risk may be huge and the feasibility may be limited if the procedures used to assess risk are expensive and require special skills.
・実現可能性と費用の課題: もし、リスク評価の手続きに費用がかかり、また特別な技能が必要となれば、リスクをスクリーニングする費用は、莫大であり、実現可能性は制限される。
In the case of dental caries this cost problem is prominent, and reinforced by the limitations of the candidate risk predictors (see Chapter 29).
齲蝕の場合、費用の課題は顕著であり、またリスク予測候補の制限は、それを増悪させる。[2009.12.30]
・Contribution to overall control of disease may be very small: the contribution of a smaller number of people at high risk of the total caries experience may be negligible compared with the burden from the many people who are at smaller risk.
・疾病全体の管理への貢献が、あまりに小さい: 齲蝕のリスクの高い人々が少なくなると、齲蝕のリスクの低い人々が増え、そこから生じる負担を比較すると、ハイリスク手法の果たす貢献は、小さくなる。
This paradox is perhaps best illustrated by the following example.
この逆説は、以下の例によく現れている。
P515
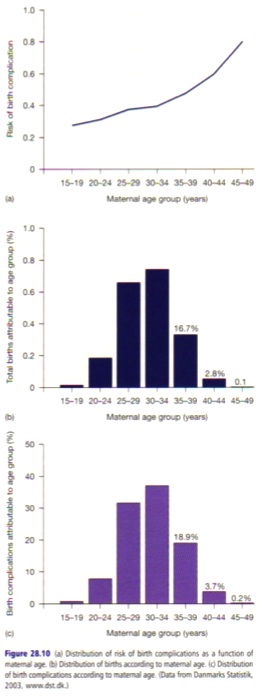
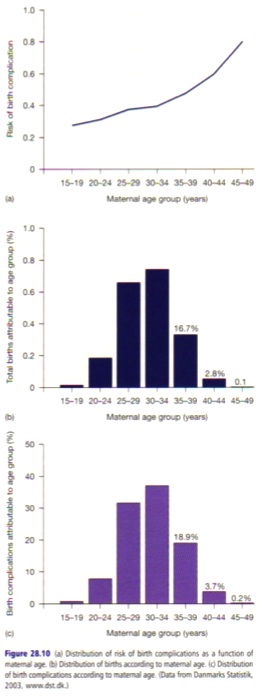 Figure28.10a shows the risk of birth complications as a function of maternal age.
Figure28.10a shows the risk of birth complications as a function of maternal age.
Figure28.10aは、 妊娠年代ごとの、出産合併症のリスクを示している。
The risk increases with age, markedly so from the age of 35 years, to reach a high of 80% at 45-49 years of age.
リスクは、加齢とともに、また35歳から目に見えて増加し、45-49歳では80%という高さに達する。
If pregnant women aged 35 years and above are considered as the target ‘high-risk’ group for birth complications, then preventive intervention would be needed in a little less than 20% of all pregnant women (Fig. 28.10b).
もし、35歳以上の女性を出産合併症の‘ハイリスク’集団として標的にするのなら、予防介入は、妊婦の20%以下が対象となるであろう (Fig. 28.10b)。
In view of the simple screening procedure (maternal age) this would be quite feasible.
(妊娠年齢という)スクリーニング手続きの簡単さから考えると、これは実用性が高い。
However, even if there existed a perfect intervention to prevent birth complications among these women, i.e. an intervention with 100% success, it would only be possible to prevent just under 23% of all cases of birth complications (Fig. 28.10c).
しかし、たとえ妊娠女性の出産合併症予防のための完璧な介入―100%予防する介入―が存在していたとしても!出産合併症全体の23%を予防するにとどまる。 (Fig. 28.10c)
This meager result arises from a combination of the smaller, but nevertheless non-zero, risk in the younger age groups and the fact that a majority of the births take place precisely in the age-groups with much smaller, non-zero risks.
この残念な結果は、小さいにせよリスク0ではない若年者と、出産の大部分は小さいにせよリスク0ではない妊娠年代で行われているという、まぎれもない事実から生じている。[2009.12.31]
For dental caries corroborating examples exist, and it has been shown that less than 6% of all new caries lesions developing over a 4-year period were found in those children who initially had been deemed at high risk, here defined as having a baseline DMFS of 7 or more (Batchelor & Sheiham, 2006).
齲蝕には、補完的な資料が存在しており、それによると、4年間以上進行するあらゆる新たなる齲蝕病巣の6%以下は、ハイリスクと判断される、つまりはじめからDMFSが7以上の小児から発生するということである (Batchelor & Sheiham, 2006)。
The vast majority of new lesions occurred in children who were caries free (DMFS = 0) at the beginning of the study.
新たなる齲蝕病巣の大部分は、齲蝕なし (DMFS=0) の小児から生じているのである。
These observations clearly indicate that the high-risk strategy may be inappropriate for caries.
これらの調査は、ハイリスク戦略は、齲蝕には適していないことを示唆している。
The population strategy for caries prevention
齲蝕予防のための集団戦略
The population strategy for prevention is particularly useful with common diseases or diseases that have widespread causes.
予防のための集団戦略は、とりわけ、蔓延する疾病あるいは原因の蔓延している疾病に有用である。
Dental caries is certainly a disease that fulfills both of these characteristics.
確かに、齲蝕はこれらの特徴を両方とも備えている。
The population strategy is based on the idea that the occurrence of disease reflects the make-up and circumstances of society as a whole.
集団戦略は、疾病の発生は社会全体の構造と環境を反映している、という概念に基づいている。
In previous sections, it has been repeatedly stressed that the nature of the direct biological causes of caries, dental plaque bacteria and fermentable carbohydrates, is dictated by oral hygiene practices and dietary habits.
前節にて、齲蝕とプラーク微生物、醗酵性炭水化物の直接の生物学的原因の性質は、口内衛生と食習慣に決定づけられていると、繰り返し強調している。
These behaviors are, in turn, socially determined, thus calling for actions at upstream levels beyond those of individual behaviors, i.e. in the social, economic, political and industrial fields.
これらの行動は、社会的に決定づけられているため、個人の行動の原因を越えた上流水準、つまり社会経済政治産業分野での活動が呼びかけられる。
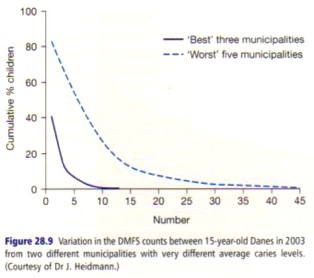 Proponents of the high-risk strategy for prevention of caries have often focussed entirely on the conspicuous right-hand tail of the distribution of caries in the population (Fig. 28.9).
Proponents of the high-risk strategy for prevention of caries have often focussed entirely on the conspicuous right-hand tail of the distribution of caries in the population (Fig. 28.9).
予防のためのハイリスク戦略の支持者は、集団における齲蝕分布で異彩を放つ右端にのみ焦点を絞っている (Fig. 28.9)。[2010.1.4]
Their objective is to truncate ― to cut off the right-hand tail ― this distribution by targeting the risk factors responsible for people being in the tail position.
ハイリスク戦略の目的は、端に位置する人々のリスク因子を標的とした、分布の右側の切り捨てである。
However, it is widely overlooked that a population-wide shift in the distribution of risk may exert a larger and longer lasting effect on the number of people falling in the right-hand tail of the distribution, because the shift of the whole population to the left pulls the right-hand tail with it.
しかし集団におけるリスク分布の変化は、分布の右端に落下する人数に大きく持続的な影響を及ぼすことを、すっかり見落としている。というのも、集団全体が左側へ移動することで、右端も左側へ引き寄せられるからだ。
A population-based approach has the additional advantage of targeting also those many who have a smaller risk and who are responsible for most of the disease cases (see Fig. 28.10a-c).
集団手法には、よりリスクの少ない、そして疾病発生の大部分と関係のある多くの人々を標的とするという、[ハイリスク手法にはない]利点がある。
P516
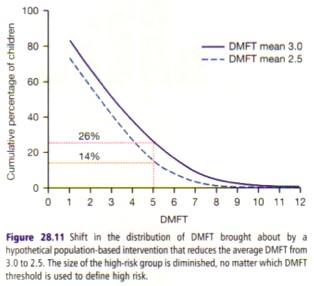
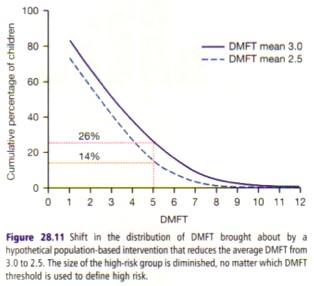 This is illustrated in Fig. 28.11, using the aforementioned observations that the distribution of DMFS or DMFT counts can be predicted on the basis of knowledge of the population mean values (Jarvinen, 1985; Batchelor & Sheiham, 2002).
This is illustrated in Fig. 28.11, using the aforementioned observations that the distribution of DMFS or DMFT counts can be predicted on the basis of knowledge of the population mean values (Jarvinen, 1985; Batchelor & Sheiham, 2002).
Fig. 28.11に、母平均の知見に基づく、DMFSカウントやDMFTカウントの分布の予測についての前述の資料を示す (Jarvinen, 1985; Batchelor & Sheiham, 2002)。
The effect was calculated of a change in the mean DMFT values from 3.0 to 2.5 on the distribution of DMFT counts that would result from a hypothetical population-based preventive strategy in a population of 12-year-olds.
予防のための集団戦略により、12歳児の集団におけるDMFT指数が3.0から2.5に低下すると仮定し、DMFTカウントの分布への影響を計算した。
Not only has this hypothetical intervention caused the prevalence of caries to decrease from 83% to 73%, but also the size of the ‘high-risk’ group has diminished.
この介入により、齲蝕有病割合は83%から73%に減少し、また‘ハイリスク’集団の規模は、 縮小すると予測された。
When an (arbitrary) cut-point of 5.0 DMFT is used to define ‘high-risk’ children, the ‘high-risk’ group has diminished from 26% to 14%, as a result of the population intervention.
(恣意的に)‘ハイリスク’児童の定義を5.0DMFTカウント以上とすると、集団介入により‘ハイリスク’集団は、全体の26%から14%に減少する。
This has occurred as a result of a shift to the left in the whole distribution, indicating lower DMFT counts for all.
これは、全体の分布が左に移動した、つまり全員のDMFTカウントが低下した結果として生じている。
The population strategy for prevention has three key advantages (Table 28.2):
予防のために集団戦略には3つの利点がある (Table 28.2)。
・It is a radical approach, because it confronts the determinants of disease at their roots, by tackling the social, economic, environmental and political circumstances that cause the biological disease determinants, i.e. the dental plaque bacteria and fermentable carbohydrates.
・集団戦略は、急進的手法である。なぜなら、集団戦略はプラーク微生物や醗酵性炭水化物といった疾病の生物学的決定
要因の原因となる社会的経済的環境に取り組むことにより、疾病の決定要因に立ち向かうからである。
・It is a potentially very powerful approach.
・集団戦略は、潜在的に強力な手法である。[2010.1.5]
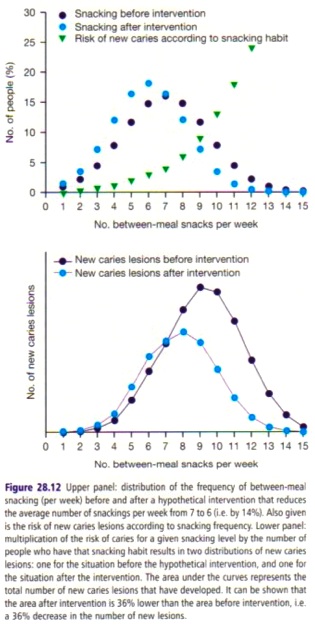
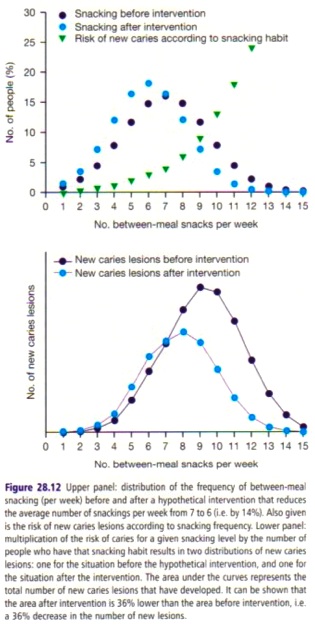 This is illustrated in Fig. 28.12, showing the effect of an achievable drop in the population distribution of the frequency of between-meal snacking from an average of seven to six between-meal snacks per week.
This is illustrated in Fig. 28.12, showing the effect of an achievable drop in the population distribution of the frequency of between-meal snacking from an average of seven to six between-meal snacks per week.
Fig. 28.12に描かれているのは、間食の平均回数を7回から6回に減らした場合の、間食回数の分布の変化とそれによる齲蝕発生にもたらされる影響である。
Using the relationship between between-meal snacking and risk of caries lesion development in the next 3 months shown in Fig. 28.12, it may be calculated that the 14% decrease in between-meal snacking will result in a 36% decrease in the total number of new caries lesions that will develop within the next 3 months.
Fig. 28.12に間食とその後3ヶ月の齲蝕進行のリスクの関係を示すが、それによると間食を14%減らすと、その後3ヶ月間に生じる新たなる齲蝕病巣の総数は36%減少するようだ。
Moreover, going back to the roots of disease has the advantage of potentially affecting a number of chronic diseases other than caries.
また、疾病の原因にさかのぼると、この効果は、齲蝕以外の慢性疾病の数に影響を及ぼす可能性もある。[2010.1.6]
Reducing between meal snacking may not only prevent caries lesions developing, but also affect obesity.
間食を節制することは、齲蝕進行を予防するだけではなく、肥満にも影響がある。
It is beyond doubt that population interventions aiming at changing people’s dietary habits in a more healthy direction away from frequent intake of high-sugar, high-fat junk foods will not only affect dental caries, but also influence the much bigger cause of population ill-health: obesity, which predisposes to cardiovascular diseases, type II diabetes, some cancers, osteoarthritis and infertility.
人々の食習慣を、砂糖過多や高脂肪なジャンクフードから、より健康的な方向へ変更することを目的とした集団介入は、齲蝕のみならず、心臓血管疾病にも影響する肥満や、2型糖尿病、がんの一部、骨関節炎、不妊症といった集団の不健康の原因にも影響をもたらす、ということには、疑う余地がない。
This is why the population strategy incorporates a common risk factor approach to prevention (Sheiham & Watt, 2000).
こういう訳で、集団戦略は、予防のための共通の危険因子手法と連携している (Sheiham & Watt, 2000)。
・The population strategy for prevention is appropriate because it acknowledges the social and contextual causes of disease (Holst et al., 2001; Newton & Bower, 2005).
・予防のための集団戦略は適切である。なぜなら、集団戦略は疾病の社会的脈絡的原因を認知している (Holst et al., 2001; Newton & Bower, 2005)。
In so doing it avoids the ‘victim-blaming’ (Chin et al., 2000; Watt, 2007) that is inherent in the ‘high-risk’ strategy, where individuals in the tails of the risk distributions are specifically targeted as if they do not belong to the parent distribution.
そのため、集団戦略は‘ハイリスク’手法に内在する‘犠牲者非難’を避ける。ハイリスク手法は、リスク分布の端の個人を、あたかも親分布に所属しないかのように、特異的に標的にする。
However, as Figs 28.9 and 28.12 clearly demonstrate, tails are intrinsic to distributions, and ‘tail-cutting’ exercises do not prevent the emergence of new cases, because the causes of the distribution have not been tackled and changed.
しかし、Fig 28.9とFig 28.12に明らかであるように、端は分布に内在しているものであり、‘しっぽ切り’は、分布の原因への取り組みではない以上、新たなる発生を予防するものではない。
Also given is the risk of new caries lesions according to snacking frequency.
ご存知とも思うが、新たなる齲蝕病巣のリスクは、間食の頻度に準じているのだ。
P517
In view of these large advantages, why is it then so difficult to convince clinicians and policy makers about the population strategy for prevention (Rose, 1992)?
これらの利点を踏まえて、予防のための集団戦略が、臨床家と政策立案者に受け入れられないのは、なぜなのだろうか (Rose, 1992)?
There are major drawbacks (Table 28.2) to the population strategy:
以下は、集団戦略の目立った欠点である。
・Limited acceptability: in general, knowledge does not cause those involved to act, unless the benefits of so doing are clearly visible, imminent and likely.
・受容性に制限がある: 一般に、行動についての知識があったとしても、その行動の恩恵が目に見えるものであり、目と鼻の先にあり、ありえそうという状況でなければ、行動にはつながらない。
People who eat ‘cariogenic’ diets will not stop this habit merely because they know about the possible consequences or are advised to do so.
‘齲蝕原性’食品を摂取する人々は、その末路について知っているというだけでは、あるいは 指導を受けたというだけでは、この習慣を止めることはない。[2010.1.6]
Faced with such advice they embark on trading-off of the personal gains against the losses associated with a change in dietary habits.
このような指導に直面すると、人々は、食習慣を変えることによる得失評価を試みる。
Their values and perceptions are frequently different from those of the dentist.
これらの得失評価の結果と理解は、しばしば、歯科医師のそれとは、異なる。
This touches on the problem of the preventive paradox (Rose, 1992): a preventive measure that may bring large benefits to the whole population may offer little benefit to each participating individual.
これは、予防の逆説の課題として説明される (Rose, 1992)。すなわち、集団に大いなる恩恵をもたらす予防施策は、しばしば、個人にはほとんど恩恵がないのだ。
The gains to be achieved for a person who reduces smoking from 10 to nine cigarettes per day are likely to be small compared with the benefits to society if smokers at large reduce smoking by this quantity.
1日あたり10本から9本に減煙する人の利得は、もし喫煙者全体がこのような減煙をすることで社会に生じる利得と比較すると、小さい。[2010.1.7]
Moreover, health professionals, such as dentists, are usually dissuaded from embarking on general healthy-diet or antismoking campaigns because they perceive their success rate to be limited, and they lack the skills and training to do so.
さらに、歯科医師のような医療従事者は、そのような運動の成功経験に乏しく、またそのための技能や訓練が足りないため、通常、全身的な健康食運動や禁煙運動を断念してしまう。
Some reluctance to act at the political level with the aim of regulating behavior may also be noted, as there is much industrial lobbying against such action.
行動規制を目的として政治水準で機能することも、そのような活動に抵抗する産業の陳情運動があるため、躊躇される。
Finally, the public may also resist such efforts, labeling them as part of the ‘nanny state.
また、世論はこのような努力に、‘過保護’とラベリングして、抵抗する。
・Feasibility: there are substantial political, economic and industrial barriers to the implementation of population preventive strategies.
・実現可能性: 予防のための集団戦略の実施には、潜在的な政治的経済的産業的障壁がある。
It is simply not in the interest of the confectionery industry to have campaigns running which aim at reducing the frequency of intake of cariogenic products in the population.
集団内の齲蝕原性製品の摂取頻度を減らすことを目的とした運動は、製菓産業の利益を損ねるだけにはとどまらない。
Moreover, there is concern that the state may lose its revenue from sugar taxation, that confectionery industry employees may lose their jobs and that advertising agencies may experience reduced turnover, if such population strategies are implemented.
このような集団戦略が実施されれば、例えば、国家は、砂糖税が減少となるし、製菓産業の被雇用者は仕事を失うし、広告代理店は減益となるだろう。
It is no wonder, therefore, that many prefer to understand individual behaviors as based on conscious and fully informed choices reflecting individual values and preferences.
それゆえ、多くの人は、個人の行動は、意識的かつ完全に個人の価値観と嗜好を反映したインフォームドチョイスに基づいていると理解したがる。
・Costs now, benefits later: it is a major barrier to the implementation of population-based preventive strategies that the costs of change, whether at the societal, industrial or individual level, must be paid now, whereas the benefits are deferred.
・投資をしても、回収までには時間がかかる: 社会であれ産業であれ個人であれ、変化への投資は、今すぐ必要であるが、回収までには時間がかかる、というのは、予防のための集団戦略の実施に立ちふさがる、大きな障壁である。
However, the rapid and impressive caries declines that many populations have witnessed over the past few decades (see Chapter 8) testify to the responsiveness of caries to changes at the population level.
ただし、ここ数十年で多くの集団に目撃された急速かつ目覚ましい齲蝕の減少(Chapter 8を見ろ)は、集団水準の変化に対する齲蝕の感応性の証拠である。
The directed population strategy
標的集団戦略
The directed population strategy combines the population and some elements of the high-risk preventive strategies in the sense that population-based methods are used to target sections of a population with a high proportion of high-risk subjects.
標的集団戦略は、ハイリスク者の割合の大きい集団を標的とした集団方法という意味で、集団戦略とハイリスク戦略の要素を組み合わせたものである。
Typically, they are populations living in geographically well-defined areas of a city (hence the alternative name of geographic targeting), known from other sources to harbor a large high-risk population (Burt, 2005).
概して、ハイリスク集団を提供する資料から分かっている都市の特定の地域(それゆえ、地理的標的とも)に住む集団を標的とする (Burt, 2005)。
This strategy thus utilizes the aforementioned variation that exists within virtually all countries and was shown in Figs 28.8 and 28.9.
それゆえ、この戦略は前述のFig 28.8と28.9にある、実質的にすべての国に存在する[地理的な]ばらつきを利用する。
From a theoretical point of view, a well-conceived directed population strategy combines the advantages of the population strategy, i.e. it is radical, powerful and appropriate, with some of the advantages of the high-risk strategy, e.g. intervention only in groups at high risk and cost-effective use of resources.
理論的な観点からは、計画性のある標的集団戦略は、急進的で強力で適切という集団戦略の利点と、ハイリスク集団のみへの介入と資源の費用効果的な活用というハイリスク戦略の利点を組み合わせたものとなる。
The directed population strategy does not screen individuals for risk.
標的集団戦略は、リスクのある個人のスクリーニングは、しない。
By targeting everybody in the area it also avoids the victim-blaming approach (Watt, 2007) inherent in the high-risk strategy.
地域の全員を標的にすることで、ハイリスク戦略に内在する犠牲者非難手法 (Watt, 2007) を避けることが出来る。[2010.1.11]
However, a major drawback is that the relatively higher cost-effectiveness of the approach may be obtained at the expense of introducing new inequities in access to health care (Tickle, 2002; Locker et al., 2004).
しかし、大きな欠点として、医療へのアクセスの新たなる不公平を招く費用から、比較的大きな費用効果が得られることがある (Tickle, 2002; Locker et al., 2004)。
Those children with substantial dental health-care needs, who happen to reside in a location designated as low risk, are less likely to obtain the dental health-care benefits they really need.
歯科医療の潜在的なニーズのある小児が、たまたまローリスクとされた地域に生活しているなら、本当に必要な歯科医療恩恵を受け損なうかもしれない。
An additional problem lies in the fact that the geodemographic distribution of caries may undermine the practicality of the directed population strategy (Tickle et al., 2003a), because the majority of the caries burden is not confined to just a small number of types of deprived areas.
さらなる課題は、齲蝕の地理的分布は、標的手段戦略の実用性を弱体化する (Tickle et al., 2003a) という事実にある。なぜなら齲蝕の負担の大部分は、いくつかの貧困地区のみに限られている訳ではないからである。
P518
A short history of caries-preventive strategies for populations
齲蝕予防の集団戦略小史
As described in detail in Chapter 18, the prominent role of fluoride in caries prevention originates with Dean’s findings during the 1930s and early 1940s of an inverse relationship between the concentration of fluoride in the drinking waters and the prevalence of dental caries (Dean et al., 1939, 1941, 1942).
Chapter 18に詳しいが、齲蝕予防におけるフッ化物の突出した働きは、1930年代と1940年代初頭に、飲料水中のフッ化物濃度と齲蝕有病割合が反比例していることを発見したDeanの功績に由来している (Dean et al., 1939, 1941, 1942)。
This observation very soon translated into public policies involving implementation of water fluoridation for caries-preventive purposes in some countries where fluoridation was technically possible (Chapter 18).
この結果は、すぐに公共政策に反映され、技術的に可能であったいくつかの国では、齲蝕予防を目的とした水道水フッ化物添加が実施された。
As expected, large caries reductions were reported, typically ranging between 40 and 70% (Burt & Fejerskov, 1996).
予想通り、大体40%から70%の範囲で、齲蝕の減少が報告された (Burt & Fejerskov, 1996)。
The percentage and actual reductions attributable to water fluoridation are much smaller now (McDonagh et al., 2000a), partly because of the impact of fluoridated toothpaste, and partly because of the diminishing returns phenomenon.
水道水フッ化物添加に起因する割合と実際の減少は、現在ではより小さくなっている (McDonagh et al., 2000a)。その理由の一部に、フッ化物配合歯磨剤の影響や齲蝕の減少がある。
Water fluoridation has been of tremendous benefit as a population strategy for caries prevention in high-caries populations, e.g. most populations before the 1980s (Burt & Fejerskov, 1996).
水道水フッ化物添加には、齲蝕好発集団、例えば1980年代以前の集団には、齲蝕予防の上で途方もない恩恵がある (Burt & Fejerskov, 1996)。
Indeed, the United States Centers for Disease Control and Prevention has listed water fluoridation among the top 10 public health achievements during the twentieth century (CDC, 1999).
いかにもCDCは、水道水フッ化物添加を、20世紀に達成された公衆衛生の10傑にあげた。
This success led to the consideration of alternative means of providing fluoride exposure to populations at large.
水道水フッ化物添加の成功は、集団全体にフッ化物を提供する、新たなる方法を検討を促すこととなった。
Such measures have included salt and milk fluoridation (Burt & Marthaler, 1996; Yeung et al., 2005), and even sugar fluoridation (Mulyani & McIntyre, 2002).
こうして検討された方法には、食塩やミルクのフッ化物添加 (Burt & Marthaler, 1996; Yeung et al., 2005)、そして砂糖のフッ化物添加 (Mulyani & McIntyre, 2002) がある。
These means provide an illustration of the potential impact of engaging industry in producing more health-promoting products.
これらの方法は、より多くの健康づくり製品を生産する産業が参入する可能性をもたらす。[2010.1.13]
Other fluoride programs aimed at populations at large include policies for the prescription of fluoride supplements (Hamasha et al., 2005), typically in the form of tablets or drops, for children living in low-fluoride areas, and the implementation of fluoride rinsing programs (Marinho et al., 2003a; Twetman et al., 2004), typically delivered in school-based settings.
そのほかの集団全体へのフッ化物計画には、低フッ化物地域の小児のためのタブレットやドロップ形態のフッ化物栄養補助剤の処方のための政策 (Hamasha et al., 2005) や、学校で提供されるフッ化物洗口計画の実施 (Marinho et al., 2003a; Twetman et al., 2004) がある。
Apart from the fluoride mouth-rinsing programs all the population strategies for caries prevention implemented from early on have involved the systemic intake of fluoride.
初期から実施されている齲蝕予防のための集団戦略は、フッ化物洗口を除けば、すべてがフッ化物の全身応用である。[2010.1.15]
However, these population strategies for caries prevention using fluoride, many of which have been in widespread use since the 1950s, have increasingly been challenged (Disney et al., 1990; Burt, 1999; McDonagh et al., 2000b; Twetman et al., 2004) on the grounds of an altered risk-benefit ratio.
しかし、これらのフッ化物を利用した齲蝕予防のための集団戦略は、その多くが1950年代から普及しているものであり、損益比の観点からは、課題のあるものとなってきている (Disney et al., 1990; Burt, 1999; McDonagh et al., 2000b; Twetman et al., 2004)。[risk-benefit ratioは、benefit-risk ratioと同義か?]
The general caries decline has resulted in a diminished effectiveness of these population prophylactic fluoride programs relative to earlier results (Hausen, 2004), while increasing concern has been voiced over the adverse effects of systemic fluoride ingestion, mainly dental fluorosis (Burt, 1999; McDonagh et al., 2000b).
現在の齲蝕減少は、集団フッ化物応用による予防計画の効果を、減じており (Hausen, 2004)、フッ化物の全身応用の副作用、ま、歯のフッ素症ですが、そのことへの危惧が高まっている。 (Burt, 1999; McDonagh et al., 2000b)
This and the increasing awareness of the posteruptive cariostatic effect of fluoride have resulted in water fluoridation occasionally even being discontinued, without a resurgence of caries (Kunzel & Fischer, 2000; KUnzel et al., 2000; Seppa et al., 2000a, b 2002; Maupome et al., 2001).
このことと、フッ化物の萌出後の抗齲蝕性への危惧は、水道水フッ化物添加を中断に追いこんでいるが、齲蝕の復活は見られない (Kunzel & Fischer, 2000; KUnzel et al., 2000; Seppa et al., 2000a, b 2002; Maupome et al., 2001)。
This is not so surprising because other substantial sources of fluorides exist, most notably fluoridated toothpastes (Twetman et al., 2003; Marinho et al., 2003b).
その他のフッ化物、とりわけフッ化物配合歯磨剤が作用している可能性が存在するため、これは驚くことではない (Twetman et al., 2003; Marinho et al., 2003b)。
Fluoridated toothpastes were first marketed in the USA in 1955 (Ellwood & Fejerskov, 2003) and they now dominate the toothpaste market in the high-income countries (Burt, 2002).
フッ化物配合歯磨剤は、USAでは1955年に発売 (Ellwood & Fejerskov, 2003) されており、現在の先進国では市場を占有している (Burt, 2002)。
While fluoridated tooth-pastes were not introduced in Denmark until 1964 (Helm & Helm, 1990), they nevertheless increased their market share to 80% in only 6 years (Helm & Helm, 1990).
デンマークではフッ化物配合歯磨剤は1964年まで販売されていなかった (Helm & Helm, 1990) が、発売後6年で市場占有率80%を占めるになった。[日本語の課題ですが、市場占有率は、率ではなく割合です。]
Today they account for more than 95% of all toothpaste sales in European countries (Arnadottir et al., 2004).
今日の欧州では、フッ化物配合歯磨剤は、歯磨剤の全売上の95%を占める (Arnadottir et al., 2004)。
There is thus no doubt that fluoridated toothpastes are a crucially important vehicle for the delivery of the caries-preventive effects of fluoride to populations at large (Seppa, 2001).
歯磨剤が集団全体へのフッ化物供給を担っていることに、疑いはない (Seppa, 2001)。
Notwithstanding this trend towards more emphasis on the intraoral delivery of fluorides, a case may still be made for the use of water fluoridation in caries prevention (Burt, 2002; Tagliaferro et al., 2004).
フッ化物供給についてのこの傾向にもかかわらず、未だに、齲蝕予防のための水道水フッ化物添加の利用については、言い分がある (Burt, 2002; Tagliaferro et al., 2004)。
For example, there are socio-economic and behavioral aspects of caries prevention by means of fluoride supplements, topical fluorides and fluoridated toothpastes that may preclude socially and materially disadvantaged population groups from enjoying the benefits of intraoral delivery of fluorides.
例えば、フッ化物栄養補助剤、フッ化物局所応用、フッ化物配合歯磨剤を用いた齲蝕予防には、社会経済的行動的な側面があるため、貧困層はフッ化物の局所供給の恩恵に浴することを社会的物質的に妨げられている。
Poor and deprived people may simply not have the material and psychosocial resources necessary to buy toothbrushes and toothpastes and to access dental health care.
貧困層の人々は、単純に、歯ブラシと歯磨剤の購入と歯科受診に必要な、物質的心理社会的資源を持っていない。[2010.1.16]
It has thus been shown that the general trend for a caries decline is less marked among non-privileged children than among their more privileged counterparts (Van Nieuwenhuysen et al., 2002), indicating an increased polarization of the caries occurrence attributable to social and material circumstances.
齲蝕減少の一般的な傾向は、非富裕層の小児には顕著ではなく (Van Nieuwenhuysen et al., 2002)、社会的物質的環境による齲蝕発生の極性形成が示唆されている。[実際にはpolarizationではなくsocial gradientかと]
As these groups are also commonly the groups that carry the more substantial part of the caries burden, water fluoridation may be a measure for reducing the social class disparities in dental caries (Burt, 2002; Tagliaferro et al., 2004).
これらの集団は、一般に、齲蝕の負担のかなりの部分を支えており、水道水フッ化物添加は、この齲蝕の社会階層による格差を緩和する (Burt, 2002; Tagliaferro et al., 2004)。
It is a caries-preventive means for reducing socioeconomic disparities in caries occurrence (Riley et al., 1999; Jones & Worthington, 1999, 2000), precisely because it is a classic population strategy.
水道水フッ化物添加は、齲蝕発生の社会経済的格差を緩和するための齲蝕予防法であり (Riley et al., 1999; Jones & Worthington, 1999, 2000)、それは古典的集団戦略だからこそ、である。
Despite the logical and obvious advantages of using a population strategy, the high-risk strategies to caries prevention are recommended by a small number of cariologists and public health dentists because of the substantial decline in caries levels and the skewed distribution of caries in high-income nations (Burt, 1998).
集団戦略の論理的かつ明確な利点にもかかわらず、齲蝕水準の大きな低下と先進国における齲蝕の傾斜分布から、齲蝕予防のためのハイリスク戦略を推奨する[とんちんかんな]齲蝕学者や公衆衛生歯科医師がいる (Burt, 1998)。
More children remain cavity free and the major proportion of the total caries burden is confined to a smaller proportion of children.
多くの小児が齲蝕なしであり、齲蝕の全負担の大部分が、一部の小児に集中している。
This has led to the questioning of the cost-effectiveness of using population strategies for caries prevention (Burt, 1998).
これは、齲蝕予防のために集団戦略を応用することの費用効果への疑問の種となっている (Burt, 1998)。
Instead, alternative approaches are suggested that specifically target those at high risk but, as outlined in this chapter and elsewhere, there are cogent arguments against using such approaches (Sheiham & Joffe, 1991; Hausen, 1997; Hausen et al., 2000; Batchelor & Sheiham, 2006).
そうはいっても、本章ほかで詳説しているように、ハイリスクを標的とする手法には、賛成しかねるだけの、しっかりとした理由がある (Sheiham & Joffe, 1991; Hausen, 1997; Hausen et al., 2000; Batchelor & Sheiham, 2006)。
P519
High-risk approaches necessarily require methods to identify those subjects who are at high risk (Hausen, 1997; Burt, 2005).
ハイリスク手法は、必然的に、ハイリスク者を同定する方法が必要となる (Hausen, 1997; Burt, 2005)。
Even though the risk-prediction methods proposed are many and varied (Powell, 1998; Messer, 2000), it remains a fact that ‘none of the reported measures for assessing caries risk was accurate enough to be relied on mechanically when targeting caries preventive measures’ (Hausen, 1997).
リスク予測方法はたくさんある (Powell, 1998; Messer, 2000) が、‘信頼に足る正確な齲蝕リスク評価方法は、ない’という事実は残ったままだ (Hausen, 1997)。
As discussed in Chapter 29, two additional requirements must be fulfilled for high-risk strategies: a sufficiently low occurrence of caries to justify the costs of screening for risk, and efficacious caries-preventive methods to offer to the high-risk subjects identified.
Chapter 29で論じるように、ハイリスク戦略は、2つの必要条件を満たさなければいけない。リスクのスクリーニングの費用を正当化するだけの十分に低い発生率と、同定されたハイリスク者に申し出る有効な齲蝕予防方法である。
As regards these requirements, there is good evidence that the high-risk strategy does not work in schoolchildren (Seppä et al., 1991; Hausen et al., 2000).
これらの必要条件に関しては、ハイリスク戦略は学童では機能しない、というすぐれた検証がある (Seppä et al., 1991; Hausen et al., 2000)。
There is some evidence that risk-based prevention involving basic prevention, sealants, chlorhexidine and fluoride varnishes at regular intervals may be effective (Pienihäkkinen et al., 2005), and under certain conditions also cost-reducing (Jokela & Pienihäkkinen, 2003), when instituted among very young (2-5-year-old) children.
定期的な基本的予防、シーラント、クロルヘキシジン、フッ化物ワニスとあわせたハイリスク予防は効果的であり (Pienihäkkinen et al., 2005)、(2-5歳児という)幼児期で特定の状況下であればコスト削減を果たす (Jokela & Pienihäkkinen, 2003) という検証もある。
However, the results of a recent high-quality clinical trial of the caries reducing effect of a combination of oral hygiene, counseling, and non-invasive caries controlling measures given to children with active non-cavitated caries lesions has shown great promise (Hausen et al., 2007).
しかし、近年の、活動性の非齲窩性齲蝕病巣のある児童に、口内衛生、食事活動、非侵襲性齲蝕管理方法を組み合わせた齲蝕予防を施すことの効果についての高品質な臨床試験は、見所のある結果を呈している (Hausen et al., 2007)。
This regimen proved able to reduce the DMFS increment among 11-12-year-old children by 44% over a 3½-year period.
この計画は、11-12歳児のDMFS増加を3年半で44%減じる可能性があることを示した。
In view of the difficulties it is perhaps not surprising that the cost-effectiveness of using a directed population strategy (geographic targeting) has received growing attention in recent years.
困難さの観点から、標的集団戦略(地理的標的)の費用効果は、近年注目となってきてきていることは、驚きではない。
The strategies evaluated for efficacy involve: supervised tooth brushing using fluoridated toothpaste among children attending schools in deprived areas (Curnow et al., 2002); fluoride varnishes given at different intervals to adolescents from socio-economically defined high-risk areas (Sköld et al., 2005); and provision of free fluoridated toothpaste and toothbrushes to children aged 1-5½ years residing in areas with different levels of material deprivation (Davies et al., 2003; Ellwood et al., 2004).
この戦略の有効性の評価は以下の通りである。貧困地域の学童の監督下でのフッ化物配合歯磨剤を利用したブラッシング (Curnow et al., 2002)。社会経済的にハイリスクとされた地域の成人への様々な感覚でのフッ化物ワニス塗布 (Sköld et al., 2005)。
物質的に貧困である地域に住む1-5歳半の幼児への無料のフッ化物配合歯磨剤と歯ブラシ配布 (Davies et al., 2003; Ellwood et al., 2004)。
While the results of the studies on the efficacy (Curnow et al., 2002; Ellwood et al., 2004; Skold et al., 2005) and cost-effectiveness (Davies et al., 2003) appear promising, it remains to be elucidated how such strategies work when attempting to extend them to all high-risk areas in a country (Tickle et al., 2003a), and to what extent subjects with high preventive needs who happen to reside in low-risk areas are indeed precluded from enjoying the benefits of the caries-preventive programs (Tickle, 2002; Locker et al., 2004).
有効性 (Curnow et al., 2002; Ellwood et al., 2004; Skold et al., 2005) と費用効果 (Davies et al., 2003) の調査結果は、頼もしいものであったが、国内のすべてのハイリスク地域に広めた場合、どのくらい機能するものなのか (Tickle et al., 2003a)、また、ローリスク地域に住む齲蝕予防ニーズの高い者は、齲蝕予防効果の恩恵から、実のところどの程度排除されるのか (Tickle, 2002; Locker et al., 2004) は、解明されていない。
A wider perspective on prevention
予防の幅広い展望
Traditionally, the literature on prevention has used a distinction among primary, secondary and tertiary levels of prevention (Leavell & Clark, 1965).
従来より、予防という言葉は、一次、二次、三次予防という区別をともなって使われてきている (Leavell & Clark, 1965)。
In this model, primary prevention encompasses activities undertaken to reduce the probability of disease occurrence (e.g. by vaccination campaigns).
この模型では、一次予防は、疾病発生の可能性を低下させるための活動(例えばワクチン運動)を強調している。
The term secondary prevention is used to describe activities that aim at early detection and treatment of disease (e.g. by means of screening for disease, such as the routine recall examination).
二次予防は、疾病の早期発見と早期治療を目的とした活動(例えば定期健診といった疾病のスクリーニング)である。
Tertiary prevention covers activities that aim at preventing disease progression or recurrence.
三次予防は、疾病の進行と再発の予防を目的とした活動を扱っている。
However, this model is entirely focussed on the expected outcomes of the preventive activities, and provides no guidance on the preventive strategies and the means and methods that may be employed.
しかし、この模型は完全に予防行動に期待されるアウトカムに焦点を絞っており、予防戦略や手段、方法の指針にはならない。
Prevention is therefore much better understood if an alternative scale of preventiveness is used, in which prevention is ranked in six levels (Table 28.3) that merge and overlap.
だから、もし予防を次第に移り変わる6つの水準に順位付けする基準 (Table 28.3) が利用されるなら、予防はよりよく理解される。
This preventive model captures much better the causal chains that explain how environmental effects may shape or influence personal behaviors affecting the biological factors that promote the development and progression of diseases.
この予防模型は、環境は、疾病の発生と進行を促進する生物学的因子に影響を与える個人の行動をどのように形作るのかを説明する、因果の連鎖をとらえている。
・Prevention level 1: the first level can be described as health promotional measures to make healthy choices the easy ones and unhealthy choices more difficult.
・予防水準1: 第1水準は、健康的な選択を易しい選択に、不健康な選択を困難な選択にする健康づくり政策として説明される。
Here, strategies seek to influence the material, social, economic and cultural circumstances that limit people’s potential for behavioral change.
ここでは、戦略は、人々の行動変容の潜在能力を制限する物質的社会的経済的文化的環境に影響を与えようとする。
The activities can be designed at several levels, including settings-based or structural levels.
この活動は、現場あるいは構造など、様々な水準で策定される。
A settings-based approach, for example, would include activities at nurseries, schools, universities, workplaces and residential homes for older people (Anonymous, 1986).
例えば、現場手法は、保育園、学校、大学、職場、高齢者のための養護施設での活動である (Anonymous, 1986)。
Structural approaches to prevention would include legislating against sugars in pediatric medicines, labeling of foods, regulations about school meals and advertising regulations.
予防のための構造手法は、小児薬に含まれる砂糖や食品のラベルを規制する立法措置や学校給食の規定、広告規制である。
The overall objective is individual behavior change, but the point of attack shifts from the individual to the environments in which people live.
その目的は、個人の行動変容であるが、攻撃対象は、個人から人々の生活する環境へ変化している。
The development of preventive programs that focus on settings or structural dimensions can influence the lives of more people and for longer periods than individually based interventions.
現場や構造に焦点を絞る予防計画は、個人への介入より、より多くの人々の生活に、より長期に影響を与える。
・Prevention level 2: the second level of prevention involves persuading people to change their behavior.
・予防水準2: 予防の第2水準は、人々が行動変容を起こすよう、説得することからなる。
This would include dissuading people from frequently ingesting so much refined sugar, and encouraging them to clean their teeth more effectively using fluoride toothpaste.
これは人々が精糖を頻繁に摂取しないように説得することや、人々がフッ化物配合歯磨剤を使って歯を効果的に清掃できるように後押しすることからなる。
Education and skill acquisition are key aspects, but it is well established that they often produce only limited or temporary success regarding the desired behavioral changes (Kay & Locker, 1996).
教育と技能獲得は、鍵となる側面であるが、彼らが、望ましい行動変容に関して限られた一時的な成功にとどまる (Kay & Locker, 1996)。
However, some evidence suggests that more success may be achieved by adopting a behavioral model that accommodates distinct stages of motivation for change, each of which may need different intervention approaches (Vallis et al., 2003; Prochaska et al., 2004).
しかし、さらなる成功は、それぞれがさまざまな介入手法を必要とする、変容のための動機の明確な段階を提供する行動模型に適応することにより達成される、と示唆する検証がある (Vallis et al., 2003; Prochaska et al., 2004)。
・Prevention level 3: the third level is early or presymptomatic diagnosis of disease: screening for early signs of dental caries.
・予防水準3: 第3水準は、疾病の早期あるいは発症前診断、齲蝕の初期徴候のスクリーニングである。
Preventive visits to dentists or hygienists to see where there is disease ― the dental check-up ― is the most common preventive activity at this level.
この水準で最も普及した予防活動は、予防受診、つまり歯科健診である。
However, the evidence for the cost-effectiveness of such routine dental checks is equivocal (Davenport et al., 2003a).
しかし、このような定期歯科健診の費用効果は、しっかりとは検証されていない (Davenport et al., 2003a)。
・Prevention level 4: the fourth level, closely related to the third, is preventive non-operative therapy.
・予防水準4: 第4水準は、第3水準と密接に関係がある、非外科的な予防療法である。
Here, efforts are made to arrest further lesion progression of early caries lesions by fluoride application combined with instruction on plaque control using fluoride toothpaste or use of fissure sealants and changing dietary habits.
ここでは、フッ化物配合歯磨剤を利用するプラークコントロールの指導、フィッシャーシーラントの利用、食習慣の変更を組み合わせたフッ化物応用により、初期の齲蝕病巣の進行を食い止める努力がなされる。
These preventive measures involve education.
これらの予防方法には、教育もある。
If the lesions have progressed beyond the point where arrest of further lesion development can be expected, operative procedures will be required.
もし病巣が、さらなる進行の停止を期待できるポイントを超えて進行しているなら、外科治療が必要だろう。
・Prevention level 5: at the fifth level, preventive non-operative dentistry therefore merges with therapeutic or operative dentistry, because early treatment of the disease may alter the life history of the disease for the better.
・予防水準5: 第5水準は、予防的非外科的歯科学であり、それゆえ治療的外科的歯科学と同化している。なぜなら、疾病の早期治療は疾病の生活史をよい方向へ変更するからだ。
・Prevention level 6: the sixth level is the detection and prevention of impacts, disability and handicap after disease has been halted.
・予防水準6: 第6水準は、疾病が食い止められた後の、影響と能力低下、社会的不利の検出と予防である。
Replacement of missing teeth and treatment of discolored teeth are examples of prevention at this level.
この水準の予防の例としては、喪失歯の置き換えと変色歯の治療がある。
P520
Dental services are primarily preoccupied with activities characterizing the higher levels, e.g. levels 5 and 6 and levels 3 and 4.
歯科医療は、はじめから、より高い水準、例えば水準5-6や水準3-4の特徴を先取りしている。
Levels 5 and 6 have a lower preventiveness rating and are predominantly palliative.
水準5-6は、予防的評価は低く、主に姑息的である。
The operative services rendered here do not prolong the survival of teeth significantly unless the dental disease rate of the individual has been changed.
個人の歯科疾病の発生率が変わらない限り、外科的医療は歯の寿命を延長しない。[発生率が「変わっても」、歯の寿命は延長しないのでは?]
Even so, preventive levels 1 and 2 have been shown to be the main factors relating to the dramatic decline in caries in the past 30 years (Nadanovsky & Sheiham, 1995), and reductions in dental caries have been greatest in countries where general health has improved most (Nadanovsky & Sheiham, 1994, 1995).
たとえそうであっても、予防水準1-2は、ここ30年の齲蝕の劇的な減少に関連する主な因子であること (Nadanovsky & Sheiham, 1995) が示されており、また、齲蝕の減少は全身の健康が大きく改善している国で、最も大きい (Nadanovsky & Sheiham, 1994, 1995)。
Wanted: a population-based common risk factor approach to prevention
求む: 集団単位の予防の共通の危険因子手法
The discussion so far has essentially considered the pros and cons of different approaches to the prevention of a single disease, in this case dental caries.
本節では、1つの疾病、この場合では齲蝕であるが、の予防へのさまざまな手法の賛否を検討する。
This focus on the prevention of single disease entities conforms to traditional dental thinking, which is largely concerned with
responding to the dental needs of individuals, in particular their dental treatment needs.
この1つの疾病そのものの予防への焦点は、従来の歯科の考え方と合致しており、個人の歯科のニーズ、とりわけ歯科治療へのニーズへ
の反応に大きく関係している。
This organ-centered thinking is not unique to the oral cavity-focussed specialty named dentistry, but also pervades medicine with all its subspecialties, e.g. ear, nose and throat, dermatology, gastroenterology and hematology.
この臓器中心思考は、口内に焦点を絞る歯科学に特有のことではなく、例えば、耳、鼻、のど、皮膚、胃腸、血液といったあらゆる下位専門分野にはびこっている。
However, the increasing realization that medical professionals need to address structural and contextual causes of diseases, rather than adhering to ‘traditional’ biological models for disease causation, implies that they need to adopt a different approach, and consider a whole range of diseases that have these causes in common.
しかし、医療従事者は、疾病の‘従来の’生物学的模型にもとづく原因に粘着するのではなく、疾病の構造的脈絡的原因を管理する必要がある、という認識の高まりは、医療従事者は異なる手法に適応し、これらの原因を共有するあらゆる疾病を考慮する必要があるということを示唆している。
When the traditional chairside preventive armamentarium, e.g. preventive check-ups, oral health education, oral hygiene instructions, dietary counseling, topical fluorides, and pit and fissure sealants (Marinho et al., 2002a, b, 2003c, d; 2004b; Davenport et al., 2003a, b; Kallestal et al., 2003; Lingstrom et al., 2003; Mejare et al., 2003; Ahovuo-Saloranta et al., 2004; Davies et al., 2005; Beirne et al., 2005), has been subjected to systematic reviews on their efficacy and cost-effectiveness, the results have all too often been disappointing.
予防健診、口内教育、口内指導、食習慣指導、局所フッ化物応用、小窩裂溝シーラント (Marinho et al., 2002a, b, 2003c, d; 2004b; Davenport et al., 2003a, b; Kallestal et al., 2003; Lingstrom et al., 2003; Mejare et al., 2003; Ahovuo-Saloranta et al., 2004; Davies et al., 2005; Beirne et al., 2005) などの従来の臨床予防活動は、その有効性と費用効果についてのシステマティックレビューにさらされており、その結果は、どれも残念なこととなっている。
The reviews indicate that there is only very limited and usually poor-quality evidence for a beneficial effect of these methods.
システマティックレビューは、これらの方法の有益な効果は、いまいちよく検証されていないことを示唆している。
While absence of evidence cannot be taken to mean evidence of absence (Altman & Bland, 1995; Alderton, 2005), the time is ripe for acknowledging that interventions of demonstrated benefit should be of higher priority, and that it ‘is no longer enough for us to faithfully believe that we are preventing disease, or promoting health, by suggesting that people reduce their sugar intake if there is no evidence that this is an effective activity’ (Kay, 1998).
検証がないということは、効果がないということが検証されていることとは異なる (Altman & Bland, 1995; Alderton, 2005) が、それと同時に、証明済みの恩恵のある介入こそ優先順位が高く、また‘もはや、有効作用についての検証がないならば、砂糖摂取を減じようという指導によって、疾病を予防したり、健康を増進したりするということを堅く信じるには足りない (Kay, 1998)’ということを認める時期が来ている。
The point made here is not to say that unlimited sugar intake would be acceptable, but to emphasize the urgent need for preventive measures for which there is evidence.
ここでのポイントは、無制限な砂糖摂取を認めることではなく、検証済みの予防方法を優先しようということである。
P521
There are thus two important lessons to be learnt.
学ぶべき、2つの重要な教訓がある。
Prevention must be applied using the common risk factor approach, just as a population-based approach to prevention must be emphasized.
予防のための集団手法を強調すると同時に、予防は共通の危険因子手法を応用すべきである。
There is overwhelming evidence that the individualized approaches to behavioral changes, e.g. by dietary counseling or reinforcement of oral hygiene procedures in single patients in the dental office setting, are largely ineffective in bringing about permanent behavioral changes (Kay & Locker, 1996).
歯科診療室での個的な食事指導や口内衛生の強化といった行動変容についての個人に合わせた手法は、永久的な行動変容をもたらす方法としては、奏効しない、という検証は山ほどある (Kay & Locker, 1996)。
That is why these behavioral changes are reinforced at regular intervals, often resulting in disappointment and frustration when the expected results do not come about (Kay, 1998).
そういう訳で、これらの行動変容は定期健診にて強化されるが、思ったような結果がでないと、しばしば失意と欲求不満に終始する (Kay, 1998)。
This limited effect is in stark contrast with the effects of institutional changes, e.g. by industry changing the composition of their products towards more health-sustaining components (fluoride in toothpastes, sugar-free confectionery, low-fat snacks, sugar-free soft drinks), or by government action (e.g. bans on smoking in public places, provision of free school meals, bans on the use of sugar in children’s medicine, decreased consumption taxes on fruits and vegetables, restrictions on aggressive advertisements for unhealthy products).
この限られた影響は、例えば企業が健康製品の組成(例えば歯磨剤中のフッ化物、砂糖なしの菓子、低脂肪スナック、砂糖なしの清涼飲料水)を変えることによる影響や、政府の活動(例えば公共の場での禁煙、学校給食の提供、小児用薬品への砂糖添加の禁止、果物と野菜への消費税減税、不健康な製品の積極的広告の制限)の影響とは対照的である。
These changes have the potential to change norms and options permanently towards the healthier choices.
これらの変化には、より健康的な選択に向かって永続的に規範と選択を変容させる可能性がある。
When such changes have been widely implemented more resources will be available to devote to the smaller subgroups that continue to require intense and individualized prevention and treatment.
このような変化が広く生じるようになれば、より多くの資源が、激しく個人的予防と治療を要求し続ける、より小さな集団に投じられるようになるだろう。
It follows from this recommendation that the interventions needed must use multiple health-promotional approaches (e.g. education, social support, laws, incentives, behavior change) to change these determinants.
それは、必要とされる介入は、決定要因に働きかける、多様な健康づくり手法(例えば教育、社会支援、法律、インセンティブ、行動変容)を利用しなければいけない、という勧告に続いて生じる。[この辺はAlma-ata Declarationのパクリか?]
Moreover, the interventions must take the long view of health outcomes, as changes often take many years to become established.
さらに、変化は、しばしば数年をかけて達成されるため、長期的視野でヘルスアウトカムを理解しなければいけない。
Finally, it is necessary that interventions involve a variety of sectors in a society that have not traditionally been associated with health-promotion efforts, including law, business, education, social services and the media (Anonymous, 1986).
そして、従来は健康づくり活動と提携していなかった、法曹界、経済界、教育界、社会奉仕界、メディア界といった、社会の多部門を巻き込んだ介入が必要である (Anonymous, 1986)。
There is no doubt that population-based strategies are here to stay and proliferate.
集団戦略が長続きし、拡散することに疑いはない。
The exponential growth in the economic burden of the hitherto predominantly palliative approaches to population health problems will eventually force attention towards tackling the root causes of diseases, if we are to continue to cope with the cumulative effects of older populations presenting with many more preventable diseases.
もし、多くのより予防可能な疾病をもつ高齢者集団が増え続けることに立ち向かうのなら、主に集団の健康課題への、今までの一時的手法による経済的負荷は指数関数的に成長し続け、そのことは最終的に、疾病の原因の原因への取り組みに注意を向けさせることとなる。
Where does this leave the traditional dentist? Need for a new professionalism
これは、どこで、従来の歯科医師を置き去りにするのか?新たなる専門性の必要性
Caries will probably continue to constitute a prevalent but not severe problem in most populations (see Chapter 8).
齲蝕は、蔓延は続くが、重大な疾病ではなくなるだろう(Chapter 8を見ろ)。
The caries decline in children and young adults may represent a delay or slowing of caries development, rather than a permanent prevention of all future caries development, for the entire lifetime (Luan et al., 2000; Hugoson et al., 2000; Griffin et al., 2005).
小児と若年者における齲蝕減少は、齲蝕進行、時期的にも速度的にも遅くなっていることを示しているが、生涯にわたり永続的に防がれるということは示していない (Luan et al., 2000; Hugoson et al., 2000; Griffin et al., 2005)。
Tooth extractions are no longer an acceptable solution to dental problems in many populations, and adult and elderly populations worldwide therefore retain increasingly more natural teeth (Kalsbeek et al., 1998; Hugoson et al., 2000, 2005; Fure, 2003; Petersen et al., 2004) and experience reducing edentulism (Ahlqwist et al., 1999; CDC, 2003; Hugoson et al., 2005).
抜歯は多くの集団において、歯の疾病の解決としては受け入れられないものとなっており、それゆえ成人と高齢者はますます天然歯を維持するようになっており (Kalsbeek et al., 1998; Hugoson et al., 2000, 2005; Fure, 2003; Petersen et al., 2004)、無歯顎の減少も生じている (Kalsbeek et al., 1998; Hugoson et al., 2000, 2005; Fure, 2003; Petersen et al., 2004)。
Evidence also points to a decline in the propensity of dentists to carry out operative caries treatments in response to their clinical observations, indicating the use of more stringent criteria for operative treatment (Heidmann et al., 1988; Gimmestad et al., 2003).
検証によると、厳しい基準で外科治療の適応について指摘する冷徹な観察者のために、齲蝕の外科的治療に対する歯科医師の性癖も衰えてきている (Heidmann et al., 1988; Gimmestad et al., 2003)。[2010.1.17]
This would in itself contribute to a lower caries occurrence (Gimmestad et al., 2003), partly by a reduction in the F component of the DMF index, and partly owing to the reduction in the D component resulting from the increased focus on non-operative treatment.
DMF指数のFを小さくするということ、そして非外科的治療に焦点を絞ることでDが小さくなるということで、これは、それ自体、齲蝕発生を少なくすることに貢献している (Gimmestad et al., 2003)。
The consequence of this development is a shift in the distribution of the caries burden, as illustrated for a Swedish population in Table 28.4.
Table 28.4のスウェーデンの状況に示されているように、この開発の帰結は、齲蝕の負担の分布の移動となった。
The table illustrates the marked change in the epidemiological characteristics of caries: the age at which people develop their (first) caries lesions is increasing, but people (at least in the high-income countries) live longer and retain many more teeth that may continue to be afflicted by caries (Schuller & Holst, 1998; Shay, 2004; Beltran-Aguilar et al., 2005).
この表は、齲蝕の疫学的性質が大きく変化していることを示している。 齲蝕病巣の初発年齢は上昇し、(少なくとも先進国の)人々は長生きするようになり、より多くの歯が齲蝕の危険にさらされるようになってきている (Schuller & Holst, 1998; Shay, 2004; Beltran-Aguilar et al., 2005)。
This results in an increasingly larger proportion of the total caries burden being found in the older sections of the population (Holst & Schuller, 2000; Beltran-Aguilar et al., 2005) (Table 28.4).
これは、齲蝕の全負担に占める高齢者の割合をますます大きくする (Holst & Schuller, 2000; Beltran-Aguilar et al., 2005) (Table 28.4)。
Concomitant with these changes, changes are also seen in the distribution of caries across socioeconomic strata: the caries decline has resulted in an altered distribution of the total caries burden (Splieth et al., 2004; Burt, 2005), such that the caries burden is increasingly polarized (Macek et al., 2004) towards less resourceful individuals from socially deprived areas or from lower socioeconomic population strata (Vargas et al., 1998; Jones & Worthington, 1999, 2000; Gillcrist et al., 2001; Manila et al., 2005; Perinetti et al., 2005).
これらの変化にともない、社会経済的階層を横断する齲蝕の分布にも変化が見られる。齲蝕の減少は齲蝕の全負担の分布を変化 (Splieth et al., 2004; Burt, 2005) させ、極性を形成し (Macek et al., 2004)、社会的な貧困地区や社会経済的な階層の低い集団から、とりわけ資源のない個人へと、齲蝕の負担が移動する (Vargas et al., 1998; Jones & Worthington, 1999, 2000; Gillcrist et al., 2001; Manila et al., 2005; Perinetti et al., 2005)。[2010.1.18]
A very strong argument for an intensified focus on caries prevention in populations is thus found in the problem of these health inequalities (Watt & Sheiham, 1999; Splieth et al., 2004; Brennan & Spencer, 2004), which traditional practice-based preventive dental services are not capable of reducing (Brennan et al., 2000; Ismail & Sohn, 2001; Tickle et al., 2002; Brennan & Spencer, 2005; Cabral et al., 2005), because people from lower socioeconomic strata may not go to the dentist until they are in pain.
集団の齲蝕予防に焦点を絞ることへの極めて強力な理由は、健康の不平等という課題 (Watt & Sheiham, 1999; Splieth et al., 2004; Brennan & Spencer, 2004)、そして社会経済的階層の低い人々は痛みなければ歯科受診をしないため、従来の臨床予防医療には健康の不平等を緩和する能力がないということ (Brennan et al., 2000; Ismail & Sohn, 2001; Tickle et al., 2002; Brennan & Spencer, 2005; Cabral et al., 2005) にある。
However, evidence suggests that the ‘poor people―poor oral health’ connection is less attributable to infrequent dental visiting and limited self-care than commonly thought (Sanders et al., 2006).
しかし、検証によれば、‘貧しい人々―劣悪な口内保健’のつながりは、一般的に思い込まれているほどには、不定期な歯科受診と低水準なセルフケアに貢献していない。
This is precisely why tackling the social gradient in oral health also necessitates focus on the social environments in which health behaviors are developed and sustained.
正確には、このような理由で、口内保健の社会的勾配に取り組むには、健康行動を確立し維持する社会環境に焦点を絞る必要がある。
P522
Traditional dental thinking is largely concerned with responding to the needs of individuals, in particular their needs for treatment.
従来の歯科的発想は、個人のニーズ、とりわけ治療のニーズに、大きく関係している。
This thinking has shaped dental ethics (responsibility for the dentally diseased person), the dental research questions (why do individuals get caries?) and the organization of the dental health services (responding to individual demand).
この考え方は、(歯科疾病のある人々への責任という)歯科倫理、(誰が齲蝕になっているのか?という)歯科研究の論点、そして(需要に応えるという)歯科医療の組織を形作っている。
While this individual thinking has its roots in the history of dentistry and represents a long-standing tradition, it is increasingly at variance with scientific knowledge as well as the expectations of societies.
この個人的な考え方は、歯科の歴史に起源があり、また長年の因習を表しているが、科学的な知見と社会の期待にはそぐわなくなってきている。
It is thus gradually realized that traditional dental thinking does not lead to the eradication of a mass disease such as dental caries.
それゆえ、徐々に、従来の歯科的思考は、齲蝕のような蔓延した疾病を根絶には導かない、と認識されてきている。
Dentistry is based on the implicit assumption that treatment of disease by dentists will achieve better oral health, and that resources will continue to be available to fund the dentists’ efforts.
歯科は、 歯科医師による疾病の治療は、口内保健を改善し、歯科医師の努力を支える持続可能な資源が存在しているという、暗黙の想定に基づいている。
However, in an era of evidence-based medicine and dentistry this assumption is no longer tenable.
しかし、検証が重視される医療と歯科医療の時代では、この想定は支持されない。
The major contribution to the reduction in caries falls outside conventional dental practice.
従来の歯科医療は、齲蝕減少に貢献していない。
This, and the relatively benign nature of caries (compared with many other threats to human health), makes it somewhat paradoxical that dental caries, unlike any other chronic human disease, requires 6-or 12-monthly surveillance and therapeutic interventions throughout life.
このことと、(そのほかの疾病と比較して)齲蝕の比較的害のない性質によって、齲蝕は、生涯にわたり、半年か一年ごとの診査と治療を必要とする。これは他の慢性疾病とは異なっており、また逆説的である。[2010.1.19]
Even though there is no evidence to support the necessity of routine 6-monthly check-ups for caries control (Davenport et al., 2003b), dental practitioners often continue to adhere to this regimen (Mettes et al., 2005), even for low-risk patients (Frame et al., 2000).
齲蝕管理のための6ヶ月健診の必要性を支持する検証はない (Davenport et al., 2003b) にもかかわらず、歯科医師はこの管理法に粘着し続け (Mettes et al., 2005)、あろうことかそれはローリスク受診者にも及ぶ (Frame et al., 2000)。
The fact that caries persists as a public health problem despite such efforts from the dental health-care system strongly suggests that current approaches to caries prevention need to be reoriented.
歯科医療制度の努力にも関わらず齲蝕は公衆衛生的課題として存在している、という事実は、現在の齲蝕予防手法は再設定される必要があることを、強く示唆している。[reorientedという表現は、Ottawa Charterのパクリ、じゃなくてリスペクトだね]
The population approach using a common risk factor approach is the orientation needed.
共通の危険因子手法を利用した集団手法が、必要とされる方向性である。
P523
In addition to the traditional focus on symptomatic relief, society at large is increasingly expecting health-care systems (including the dental care systems) to engage in disease prevention, show solidarity with the weaker in society, acting against inequalities, and contributing to increasing the population’s sense of security and quality of life and well-being (Holmstrup & Rossel, 2000; Benn, 2003).
従来の症候性の不安への焦点に加えて、社会全体はますます、医療制度(歯科医療含む)が、疾病予防を組み込み、社会の弱者と手を携え、不平等に立ち向かい、人々の安心感と生活の質、快適な暮らしの改善に貢献することを、期待している。
Dentistry has a long history of exercising paternalism and remains largely unregulated as to the appropriateness of the treatments provided (Friedman & Atchison, 1993; Hartshorne & Hasegawa, 2003), an approach that engenders public distrust (Ecenbarger, 1997).
歯科学には、パターナリスムの行使の長い歴史があり、治療提供の適切性 (Friedman & Atchison, 1993; Hartshorne & Hasegawa, 2003) と国民の不信感を生む手法 (Ecenbarger, 1997) に関しては、概ね統制がない。
Society at large is therefore increasingly asking for accountability, transparency and sound professional standards (Cruess et al., 2000, 2002).
だから社会全体は、まずます、説明責任、透明性そして正常な職業上の基準を求めている (Cruess et al., 2000, 2002)。
In these respects the dental profession may have a long way to go.
これらを考慮すると、歯科の専門性は、ずいぶん遠くにあるようだ。
The future of the traditional dentist is under scrutiny and criticism, owing to the increasing maintenance care caries burden (e.g. replacement of restorations, endodontic treatment) in the aging sections of many populations.
従来の歯科医師の将来は、多くの集団の高齢者で増加するメインテナンス治療と齲蝕の負担(例えば、修復物の再治療や歯内療法)のせいで、精査と批判の的となる。
Therefore, dentistry should engage in a new professionalism (Friedman & Atchison, 1993; Cruess et al., 2000, 2002; Holst et al., 2002).
それゆえ、歯科は新たなる専門性を携えるべきである (Friedman & Atchison, 1993; Cruess et al., 2000, 2002; Holst et al., 2002)。
Even though traditional dental services may be necessary for some time, in the long run there will be a need for fewer and simpler procedures (Eklund, 1999), but of higher quality.
従来の歯科医療は、時には必要かもしれないが、結局はより少なくて単純 (Eklund, 1999)、そしてより高品質な処置が必要とされるようになる。
Dentists will increasingly be expected to engage in advising patients about the risks to their dental or general health, and in the investigation and control of these risks.
歯科医師は、ますます患者に歯と全身の健康へのリスクを伝えることを、そしてこれらのリスクの管理と調査を期待されるだろう。
Dentists should continue to strive to influence the behavior of patients, and perform early diagnosis of incipient disease.
歯科医師は、患者の行動に影響を与える努力を続け、疾病の早期診断を遂行すべきである。
The more crucial role of dentists in oral health promotion and caries prevention will be as health advocates.
口内の健康づくりと齲蝕予防において、より重大な役割は、健康の推進者であることである。
Health advocacy is the actions of health professionals and others with perceived expertise and authority in health issues to influence the decisions and actions of government, communities and individuals in a way that promotes health.
健康の推奨は、政府、地域、個人の決定と活動に、健康を改善するように、影響をもたらすための、認知された保健の専門家と権威、そして医療従事者とその他の人々の活動である。
Health advocacy involves a contribution to the education of the decision makers in government, communities and the media about health issues, as well as a contribution to the setting of political agendas aiming to improve the health of populations.
健康の推奨とは、政府の政策決定者、地域、健康メディアの教育に貢献し、また集団の健康の改善を目的とした政治課題の現場に貢献することである。
Dentists must come out of their four-walled offices and use their new professionalism to engage in setting the public health agenda.
歯科医師は、四壁性の診療室から抜け出して、公衆衛生政策の設定に従事することで新たなる専門性を発揮すべき、なのかもしれない。[2010.1.20]
References
Ahlqwist M, Bengtsson C, Hakeberg M, Hagglin C. Dental status of women in a 24-year longitudinal and cross-sectional study. Results from a population of women in Goteborg. Acta Odontol Scand 1999; 57: 162-7.
Ahovuo-Saloranta A, Hiiri A, Nordblad A, Worthington H, Makela M. Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents [review]. Cochrane Database of Systematic Reviews 2004; Issue 3: Art. No: CD001830.pub2. DOI: 10.1002/14651858. CD001830.pub2.
Alderton P. Absence of evidence is not evidence of absence. BMJ 2005; 328: 476-7.
Altman DG, Bland JM. Absence of evidence is not evidence of absence. BMJ 1995; 311: 485.
Anonymous. Ottawa charter for health promotion. Can J Publ Health 1986; 77: 425-30.
Anusavice KJ. Present and future approaches for the control of caries. J Dent Educ 2005; 69: 538-54.
Arnadottir IB, Ketley CE, van Loveren C, et al. A European perspective on fluoride use in seven countries. Community Dent Oral Epidemiol 2004; 32 (Suppl 1): 69-73.
Batchelor P, Sheiham A. The limitations of a `high-risk' approach for the prevention of dental caries. Community Dent Oral Epidemiol 2002; 30: 302-12.
Batchelor P, Sheiham A. The distribution of burden of dental caries in schoolchildren: a critique of the high risk caries prevention strategy for populations. BMC Oral Health 2006; 6: 3.
Beirne P, Forgie A, Clarkson JE, Worthington HV. Recall intervals for oral health in primary care patients [review]. Cochrane Database of Systematic Reviews 2005; Issue 2: Art. No.: CD004346.pub2. DOI: 10.1002/ 14651858.CD004346.pub2.
Beltran-Aguilar ED, Barker LK, Canto MT, et al. Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis - United States 1988-1994 and 1999-2002. MMWR Morb Mortal Wkly Rep 2005; 54 (no. SS-3): 1-48.
Benn DK. Professional monopoly, social covenant, and access to oral health care in the United States. J Dent Educ 2003; 67: 1080-90.
Brennan DS, Spencer AJ. Diagnostic and preventive service trends in private general practice: 1983-1984 to 1998-1999. Aust Dent J 2003a; 48: 43-9.
Brennan DS, Spencer AJ. Provision of diagnostic and preventive services in general dental practice. Community Dent Health 2003b; 20: 5-10.
Brennan DS, Spencer Al. Changes in caries experience among Australian public dental patients between 1995/96 and 2001/02. Aust N Z J Public Health 2004; 28: 542-8.
Brennan DS, Spencer AJ. The role of the dentist, practice and patient factors in the provision of dental services. Community Dent Oral Epidemiol 2005; 33: 181-95.
Brennan D, Spencer AJ, Szuster F. Service provision trends between 1983-84 and 1993-94 in Australian private general practice. Aust Dent J 1998; 43: 331-6.
Brennan DS, Spencer AJ, Szuster FSP. Service provision patterns by main diagnoses and characteristics of patients. Community Dent Oral Epidemiol 2000; 28: 225-33.
Brunner E, Marmot M. Social organization, stress, and health. In: Marmot M, Wilkinson RG, eds. Social determinants of health. Oxford: Oxford University Press, 1999. 17-43.
Burt BA. Prevention policies in the light of the changed distribution of dental caries. Acta Odontol Scand 1998; 56: 179-86. Burt BA. The case for eliminating the use of dietary fluoride supplements for young children. J Publ Health Dent 1999; 59: 269-74.
Burt BA. Fluoridation and social equity. J Publ Health Dent 2002; 62: 195-200. Burt BA. Concepts of risk in dental public health. Community Dent Oral Epidemiol 2005; 33: 240-7.
Burt BA, Fejerskov O. Water fluoridation. In: Fejerskov 0, Ekstrand J, Burt BA, eds. Fluoride in dentistry, 2nd edn. Copenhagen: Munksgaard, 1996: 275-90.
Burt BA, Marthaler TM. Fluoride tablets, salt fluoridation, and milk fluoridation. In: Fejerskov 0, Ekstrand J, Burt BA, eds. Fluoride in dentistry, 2nd edn. Copenhagen: Munksgaard, 1996: 291-310.
Cabral ED, Caldas AF Jr, Cabral HAM. Influence of the patient's race on the dentist's decision to extract or retain a decayed tooth. Community Dent Oral Epidemiol 2005; 33: 461-6.
Centers for Disease Control and Prevention (CDC). Ten great public health achievements - United States, 1900-1999. MMWR Morb Mortal Wkly Rep 1999; 48: 241-3.
Centers for Disease Control and Prevention (CDC). Public health and aging: retention of natural teeth among older adults - United States 2002. MMWR Morb Mortal Wkly Rep 2003; 52: 1226-9.
Chin NP, Monroe A, Fiscella K. Social determinants of (un)healthy behaviors. Educ Health 2000; 13: 317-28.
Cleaton-Jones P, Fatti P. Dental caries trends in Africa. Community Dent Oral Epidemiol 1999; 27: 316-20.
Cruess RL, Cruess SR, Johnston SE. Professionalism: an ideal to be sustained. Lancet 2000; 356: 156-9.
Cruess SR, Johnston S, Cruess RL. Professionalism for medicine: opportunities and obligations. Med JAust 2002; 177: 208-11.
Curnow MMT, Pine CM, Burnside G, Nicholson JA, Chesters RK, Huntington E. A randomised controlled trial of the efficacy of supervised toothbrushing in high-caries-risk children. Caries Res 2002; 36: 294-300.
Davenport C, Elley K, Salas C, et al. The clinical effectiveness and costeffectiveness of routine dental checks: a systematic review and economic evaluation. Health Technol Assess 2003a; 7(7).
Davenport CF, Elley KM, Fry-Smith A, Taylor-Weetman CL, Taylor RS. The effectiveness of routine dental checks: a systematic review of the evidence base. Br Dent J 2003b; 195: 87-98.
Davies GM, Worthington HV, Ellwood RP, et al. An assessment of the cost effectiveness of a postal toothpaste programme to prevent caries among five-year-old children in the North West of England. Community Dent Health 2003; 20: 207-10.
Davies MJ, Spencer AJ, Slade GD. Trends in dental caries experience of school children in Australia - 1977 to 1993. Aust Dent 11997; 42: 389-94.
Davies RM, Davies GM, Ellwood RP, Kay EJ. Prevention. Part 4: Toothbrushing: what advice should be given to patients? Br Dent J2005; 195: 135-41.
Dean HT, Jay P, Arnold FA Jr, McClure FJ, Elvove E. Domestic water and dental caries, including certain aspects of oral L. acidophilus. Public Health Rep 1939; 54: 862-88.
Dean HT, Jay P, Arnold FA Jr, Elvove E. Domestic water and dental caries. II. A study of 2,832 white children aged 12-14 years, of eight suburban Chicago communities, including L. acidophilus studies of 1,761 children. Public Health Rep 1941; 56: 761-92.
Dean HT, Arnold FA Jr, Elvove E. Domestic water and dental caries. V. Additional studies of the relation of fluoride domestic waters to dental caries experience in 4,425 white children aged 12-14 years of 13 cities in 4 states. Public Health Rep 1942; 57: 1155-79.
Disney JA, Bohannan HM, Klein SP, Bell RM. A case study in contesting the conventional wisdom: school-based fluoride mouthrinse programs in the USA. Community Dent Oral Epidemiol 1990; 18: 46-56.
Domejean-Orliaguet S, Tubert-Jeannin S, Riordan PJ, Espelid I, Tveit AB. French dentists' restorative treatment decisions. Oral Health Prev Dent 2004; 2: 125-31.
Downer MC. Time trends in caries experience of children in England and Wales. Caries Res 1992; 26: 466-72.
Ecenbarger W. How honest are dentists? Readers Digest 1997; February: 50-6. Eklund SA. Changing treatment patterns. J Am Dent Assoc 1999; 130: 1707-12.
Eklund SA, Pittman JL, Heller KE. Professionally applied topical fluoride and restorative care in insured children. J Public Health Dent 2000; 60: 33-8.
Ekstrand KR, Christiansen MEC, Qvist V. Influence of different variables on the inter-municipality variation in caries experience in Danish adolescents. Caries Res 2003; 37: 130-41.
Elderton RJ, Eddie S. The changing pattern of treatment in the General Dental Service 1965-1981. Part 2 - Restorative treatment and implications for the future. Br Dent J 1983; 155: 421-3.
Elderton RJ, Eddie S. Uptake of General Dental Service treatment in GreatBritain 1965-1983 with special reference to radiography, prosthetics and the care of children. Br Dent J 1986; 161: 93-8.
Ellwood R, Fejerskov O. Clinical use of fluoride. In: Fejerskov 0, Kidd E, eds. Dental caries: the disease and its clinical management. Oxford: Blackwell Munksgaard, 2003: 189-222.
Ellwood RP, Davies GM, Worthington HV, Blinkhorn AS, Taylor GO, Davies RM. Relationship between area deprivation and the anticaries benefit of an oral health programme providing free fluoride toothpaste to young children. Community Dent Oral Epidemiol 2004; 32: 159-65.
Eriksen HM. Has caries merely been postponed? Acta Odontol Scand 1998; 56: 173-5.
Fejerskov 0, Kidd EAM. Clinical cariology and operative dentistry in the twenty-first century. In: Fejerskov 0, Kidd E, eds. Dental caries. The disease and its clinical management, 1st edn. Oxford: Blackwell Munksgaard, 2003: 3-6.
Fejerskov 0, Manji F. Reactor paper: Risk assessment in dental caries. In: Bader JD, ed. Risk assessment in dentistry. Chapel Hill, NC: University of North Carolina Dental Ecology, 1990.215-17.
Fejerskov 0, Baelum V, Luan W-M, Manji E Caries prevalence in Africa and the People's Republic of China. Int Dent J 1994; 44: 425-33.
Frame PS, Sawai R, Bowen WH, Meyerowitz C. Preventive dentistry: practitioners' recommendations for low-risk patients compared with scientific evidence and practice guidelines. Am J Prev Med 2000; 18: 159-62.
Friedman JW, Atchison KA. The standard of care: an ethical reponsibility of public health dentistry. J Public Health Dent 1993; 53: 165-9.
Fure S. Ten-year incidence of tooth loss and dental caries in elderly Swedish individuals. Caries Res 2003; 37: 462-9.
Gillcrist JA, Brumley DE, Blackford JU. Community socioeconomic status and children's dental health. JAm Dent Assoc 2001; 132: 216-22.
Gimmestad AL, Holst D, Fylkenes K. Changes in restorative caries treatment in 15-year-olds in Oslo, Norway, 1979-1996. Community Dent Oral Epidemiol 2003; 31: 246-51.
Grembowski D, Milgrom P. The influence of dentist supply on the relationship between fluoridation and restorative care among children. Med Care 1988; 26: 907-17.
Grembowski D, Fiset L, Milgrom P, Conrad D, Spadafora A. Does fluoridation reduce the use of dental services among adults? Med Care 1997; 35: 454-71.
Griffin SO, Griffin PM, Swann JL, Zlobin N. New coronal caries in older adults: implications for prevention. J Dent Res 2005; 84: 715-20.
Grytten J. The effect of supplier inducement on Norwegian dental services; some empirical findings based on a theoretical model. Community Dent Health 1991; 8: 221-31.
Hamasha AA, Levy SM, Broffitt B, Warren JJ. Patterns of dietary fluoride supplement use in children from birth to 96 months of age. J Public Health Dent 2005; 65: 7-13.
Hartshorne J, Hasegawa TK. Overservicing in dental practice - ethical perspectives. J S Afr Dent Assoc 2003; 58: 364-9.
Hausen H. Caries prediction - state of the art. Community Dent Oral Epidemiol 1997; 25: 87-96.
Hausen H. How to improve the effectiveness of caries-preventive pro-grams based on fluoride. Caries Res 2004; 38: 263-7.
Hausen H, Karkkainen S, Seppa L. Application of the high-risk strategy to control dental caries. Community Dent Oral Epidemiol 2000; 28: 26-34.
Hausen H, Seppa L, Poutanen R, Niinimaa A, Lahti S, Karkkainen S, Pietila I. Noninvasive control of dental caries in children with active initial lesions. A randomized clinical trial. Caries Res 2007; 41: 384-91.
Hawkins R, Locker D, Noble J, Kay EJ. Prevention. Part 7: Professionally applied topical fluorides for caries prevention. Br Dent 1 2003; 195: 313-17.
Heidmann J, Helm S, Helm T, Poulsen S. Changes in prevalence of approximal caries in 17-year-olds and related restorative treatment strategies over a 6-year period. Community Dent Oral Epidemiol 1988; 16: 167-70.
Heller KE, Burt BA, Eklund SA. Sugared soda consumption and dental caries in the United States. J Dent Res 2001; 80: 1949-53.
Helm S, Helm T. Caries among Danish schoolchildren in birth-cohorts 1950-78. Community Dent Oral Epidemiol 1990; 18: 66-9.
Holmstrup P, Rossel P. Tandlaegeetik i ar 2000 - og fremover. Odontologi 2000. Copenhagen: Munksgaard, 2000: 23-38.
Holst D. Causes and prevention of dental caries: a perspective on cases and incidence. Oral Health Prev Dent 2005; 3: 9-14.
Holst D, Schuller AA. Oral health changes in an adult Norwegian population: a cohort analytical approach. Community Dent Oral Epidemiol 2000; 28: 102-11.
Holst D, Schuller AA, Aleksejuniene J, Eriksen HM. Caries in populations: a theoretical, causal approach. Eur J Oral Sci 2001; 109: 143-8.
Holst D, Sheiham A, Petersen PE. Regulating entrepreneurial behaviour in oral health care services. In: Saltman RB, Busse R, Mossialos E, eds. Regulating entrepreneurial behaviour in European health care systems. Buckingham: Open University Press, 2002. 215-31.
Hudson P. Conservative treatment of the class I lesion. A new paradigm for dentistry. JAm Dent Assoc 2004; 135: 760-4.
Hugoson A, Koch G, Slotte C, Bergendal T, Thorstensson B, Thorstensson H. Caries prevalence and distribution in 20-80-year-olds in Jonkoping, Sweden, in 1973, 1983, and 1993. Community Dent Oral Epidemiol 2000; 28: 90-6.
Hugoson A, Koch G, Gothberg C, et al. Oral health of individuals aged 3-80 years in Jonkoping, Sweden during 30 years (1973-2003). II. Review of clinical and radiographic findings. Swed Dent J 2005; 29: 139-55.
Ismail AI. Clinical diagnosis of precavitated carious lesions. Community Dent Oral Epidemiol 1997; 25: 13-23.
Ismail AI, Sohn W. The impact of universal access to dental care on dis- parities in caries experience in children. J Am Dent Assoc 2001; 132: 295-303.
Jarvinen S. Epidemiologic characteristics of dental caries: relation of DMFT and DMFS to proportion of children with DMF teeth. Community Dent Oral Epidemiol 1985; 13: 235-7.
Jarvis MJ, Wardle J. Social patterning of individual health behaviours: the case of cigarette smoking. In: Marmot M, Wilkinson RG, eds. Social determinants of health. Oxford: Oxford University Press, 1999. 240-55.
Jokela J, Pienihakkinen K. Economic evaluation of a risk-based caries prevention program in preschool children. Acta Odontol Scand 2003; 61: 110-14.
Jones CM, Worthington H. The relationship between water fluoridation and socioeconomic deprivation on tooth decay in 5-year-old children. Br Dent J 1999; 186: 397-400.
Jones CM, Worthington H. Water fluoridation, poverty and tooth decay in 12-year-old children. J Dent 2000; 28: 389-93.
Kallestal C, Wang NJ, Petersen PE, Arnadottir IB. Caries-preventive methods used for children and adolescents in Denmark, Iceland, Norway and Sweden. Community Dent Oral Epidemiol 1999; 27: 144-51.
Kallestal C, Norlund A, Soder B, et al. Economic evaluation of dental caries prevention: a systematic review. Acta Odontol Scand 2003; 61: 341-6.
Kalsbeek H, Truin GJ, van Rossum GMJM, van Rijkom HM, Poorterman JHG, Verrips GH. Trends in caries prevalence in Dutch adults between 1983 and 1995. Caries Res 1998; 32: 160-5.
Kay El. Caries prevention - based on evidence? Or an act of faith? Br Dent J 1998; 185: 432-3.
Kay EJ, Locker D. Is dental health education effective? A systematic review of current evidence. Community Dent Oral Epidemiol 1996; 24: 231-5.
Keyes PH. The infectious and transmissible nature of experimental dental caries. Findings and implications. Arch Oral Biol 1960; 1: 304-20.
Kumanyika S, Jeffery RW, Morabia A, Ritenbaugh C, Antipatis VJ. Obesity prevention: the case for action. Int J Obes 2002; 26: 425-36.
Kunzel W, Fischer T. Caries prevalence after cessation of water fluoridation in La Salud, Cuba. Caries Res 2000; 34: 20-5.
Kunzel W, Fischer T, Lorenz R, Bruhmann S. Decline of caries prevalence after the cessation of water fluoridation in the former East Germany. Community Dent Oral Epidemiol 2000; 28: 382-9.
Leavell HR, Clark EG. Preventive medicine for the doctor in his community; an epidemiologic approach, 3rd edn. New York: McGraw-Hill, 1965.
Lingstrom P, Holm A-K, Mejare I, et al. Dietary factors in the prevention of dental caries: a systematic review. Acta Odontol Scand 2003; 61: 331-40.
Locker D, Jokovic A, Kay El. Prevention. Part 8: The use of pit and fissure sealants in preventing caries in the permanent dentition of children. Br Dent J2003; 195: 375-8.
Locker D, Frosina C, Murray H, Wiebe D, Wiebe P. Identifying children with dental care needs: evaluation of a targetted school-based dental screening program. J Public Health Dent 2004; 64: 63-70.
Luan W-M, Baelum V, Fejerskov 0, Chen X. Ten-year incidence of dental caries in adult and elderly Chinese. Caries Res 2000; 34: 205-13.
McDonagh M, Whiting P, Bradley M, et al. A systematic review of public water fluoridation. University of York: NHS Centre for Reviews and Dissemination, 2000a: 1-100.
McDonagh MS, Whiting PF, Wilson PM, et al. Systematic review of water fluoridation. BMJ 2000b; 321: 855-9.
Macek MD, Heller KE, Selwitz RH, Manz MC. Is 75 percent of caries really found in 25 percent of the population? J Public Health Dent 2004; 64: 20-5.
McMichael AJ. The health of persons, populations, and planets: epidemiology comes full circle. Epidemiology 1995; 6: 633-6.
Marinho VCC, Higgins JPT, Logan S, Sheiham A. Fluoride gels for preventing dental caries in children and adolescents [review]. Cochrane Database of Systematic Reviews 2002a; Issue 1: Art. No.: CD002280. DOI: 10.1002/14651858.CD002280.
Marinho VCC, Higgins JPT, Logan S, Sheiham A. Fluoride varnishes for preventing dental caries in children and adolescents [review]. CochraneDatabase of Systematic Reviews 2002b; Issue 1: Art. No.: CD002279. DOI: 10.1002/ 14651858.CD002279.
Marinho VCC, Higgins JPT, Logan 5, Sheiham A. Fluoride mouthrinses for preventing dental caries in children and adolescents [review]. Cochrane Database of Systematic Reviews 2003a; Issue 3: Art. No.: CD002284. DOI: 10.1002/ 14651858.CD002284.
Marinho VCC, Higgins JPT, Logan S, Sheiham A. Fluoride toothpastes for preventing dental caries in children and adolescents [review]. Cochrane Database of Systematic Reviews 2003b; Issue 1: Art. No.: CD002278. DOI: 10.1002/ 14651858.CD002278.
Marinho VCC, Higgins JPT, Logan S, Sheiham A. Systematic review of controlled trials on the effectiveness of fluoride gels for the prevention of dental caries in children. J Dent Educ 2003c; 67: 448-58.
Marinho VCC, Higgins JPT, Logan S, Sheiham A. Topical fluoride (tooth- pastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents [review]. Cochrane Database of Systematic Reviews 2003d; Issue 4: Art. No.: CD002782. DOI: 10.1002/14651858. CD002782.
Marinho VCC, Higgins JPT, Sheiham A, Logan S. Combinations of topical fluoride (toothpastes, mouthrinses, gels, varnishes) versus single topical fluoride for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2004a; Issue 1: Art. No.: CD002781. DOI: 10.1002/ 14651858.CD002781.pub2.
Marinho VCC, Higgins JPT, Sheiham A, Logan S. One topical fluoride (toothpastes, or mouthrinses, or gels, or varnishes) versus another for preventing dental caries in children and adolescents. Cochrane Database of Systematic Reviews 2004b; Issue 1: Art. No.: CD002780. DOI: 10.1002/ 14651858.CD002780.pub2.
Marthaler TM, O'Mullane DM, Vrbic V. The prevalence of dental caries in Europe 1990-1995. Caries Res 1996; 30: 237-55.
Mattila M-L, Rautava P, Aromaa M, et al. Behavioural and demographic factors during early childhood and poor dental health at 10 years of age. Caries Res 2005; 39: 85-91.
Maupome G, Clark DC, Levy SM, Berkowitz J. Patterns of dental caries following the cessation of water fluoridation. Community Dent Oral Epidemiol 2001; 29: 37-47.
Mejare I, Lingstrom P, Petersson LG, et al. Caries-preventive effect of fissure sealants: a systematic review. Acta Odontol Scand 2003; 61: 321-30.
Messer LB. Assessing caries risk in children. Aust Dent J 2000; 45: 10-16.
Mettes TG, Bruers JJM, van der Sanden WJM, et al. Routine oral examinations: differences in characteristics of Dutch general dental practitioners related to type of recall interval. Community Dent Oral Epidemiol 2005; 33: 219-26.
Mulyani D, McIntyre J. Caries inhibitory effect of fluoridated sugar in a trial in Indonesia. Aust Dent J 2002; 47: 314-20.
Nadanovsky P, Sheiham A. The relative contribution of dental services to the changes and geographical variations in caries status of 5- and 12-year-old children in England and Wales in the 1980s. Community Dent Health 1994; 11: 215-23.
Nadanovsky P, Sheiham A. Relative contribution of dental services to the changes in caries levels of 12-year-olds children in 18 industrialized countries in the 1970s and early 1980s. Community Dent Oral Epidemiol 1995; 23: 331-9.
Newton JT, Bower El. The social determinants of oral health: new approaches to conceptualizing and researching complex causal networks. Community Dent Oral Epidemiol 2005; 33: 25-34.
Pearce N. Traditional epidemiology, modern epidemiology, and public health. Am J Public Health 1996; 86: 678-83.
Perinetti G, Caputi S, Varvara G. Risk/prevention indicators for the prevalence of dental caries in schoolchildren: results from the Italian OHSAR survey. Caries Res 2005; 39: 9-19.
Petersen PE, Kjoller M, Christensen LB, Krustrup U. Changing dentate status of adults, use of dental health services, and achievement of national dental health goals in Denmark by the year 2000. J Public Health Dent 2004; 64: 127-35.d
Pienihakkinen K, Jokela J, Alanen P. Risk-based early prevention in comparison with routine prevention of dental caries: a 7-year follow-up of a controlled clinical trial; clinical and economic aspects. BMC Oral Health 2005; 5: 2. Powell LV. Caries prediction: a review of the literature. Community Dent Oral Epidemiol 1998; 26: 361-71.
Prochaska JO, Velicer WF, Prochaska JM, Johnson JL. Size, consistency, and stability of stage effects for smoking cessation. Addict Behav 2004; 29: 207-13.
Riley JC, Lennon MA, Ellwood RP. The effect of water fluoridation and social inequalities on dental caries in 5-year-old children. Int J Epidemiol 1999; 28: 300-5.
Rose G. Sick individuals and sick populations. Int J Epidemiol 1985; 14: 32-8.
Rose G. The strategy of preventive medicine. Oxford: Oxford University Press, 1992: 1-138.
Sanders AE, Spencer AJ, Slade GD. Evaluating the role of dental behaviour in oral health inequalities. Community Dent Oral Epidemiol 2006; 34: 71-9.
Schuller AA, Holst D. Changes in the oral health status of adults from Trendelag, Norway, 1973-1983-1994. Community Dent Oral Epidemiol 1998; 26: 201-8.
Seppa L. The future of preventive programs in countries with different systems of dental care. Caries Res 2001; 35(Suppl 1): 26-9. Seppa L. Fluoride varnishes in caries prevention. Med Princ Pract 2004; 13: 307-11.
Seppa L, Hausen H, Pollanen L, Karkkainen S, Helasharju K. Effect of intensified caries prevention on approximal caries in adolescents with high caries risk. Caries Res 1991; 25: 392-5.
Seppa L, Karkkainen S, Hausen H. Caries in the primary dentition, after discontinuation of water fluoridation, among children receiving comprehensive dental care. Community Dent Oral Epidemiol 2000a; 28: 281-8.
Seppa L, Karkkainen S, Hausen H. Caries trends 1992-1998 in two low- fluoride Finnish towns formerly with and without fluoridation. Caries Res 2000b; 34: 462-8.
Seppa L, Hausen H, Karkkainen S, Larmas M. Caries occurrence in a fluoridated and a nonfluoridated town in Finland: a retrospective study using longitudinal data from public health records. Caries Res 2002; 36: 308-14.
Shay K. The evolving impact of aging America on dental practice. I Contemp Dent Pract 2004; 5: 101-10.
Sheiham A. Impact of dental treatment on the incidence of dental caries in children and adults. Community Dent Oral Epidemiol 1997; 25: 104-12.
Sheiham A, Joffe M. Public dental health strategies for identifying and controlling dental caries in high and low risk populations. In: Johnson NW, ed. Risk markers for oral diseases. Vol. 1, Dental caries. Markers of high and low risk groups and individuals. Cambridge: Cambridge University Press, 1991: 445-81.
Sheiham A, Watt RG. The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol 2000; 28: 399-406.
Skold UM, Petersson LG, Lith A, Birhhed D. Effect of school-based fluoride varnish programmes on approximal caries in adolescents from dif- ferent caries risk areas. Caries Res 2005; 39: 273-9.
Splieth CH, Nourallah AW, Konig KG. Caries prevention programs for groups: out of fashion or up to date? Clin Oral Invest 2004; 8: 6-10.
Tagliaferro EPS, Cypriano S, Sousa MLR, Wada RS. Caries experience among schoolchildren in relation to community fluoridation status and town size. Acta Odontol Scand 2004; 62: 124-8.
Tickle M. The 80:20 phenomenon: help or hindrance to planning caries prevention programmes? Community Dent Health 2002; 19: 39-42.
Tickle M, Milsom KM, Blinkhorn AS. Inequalities in the dental treatment provided to children: an example from the UK. Community Dent Oral Epidemiol 2002; 30: 335-41.
Tickle M, Milsom KM, Jenner TM, Blinkhorn AS. The geodemographic distribution of caries experience in neighboring fluoridated and nonfluoridated populations. I Public Health Dent 2003a; 63: 92-8.
Tickle M, Milsom KM, King D, Blinkhorn AS. The influences on preventive care provided to children who frequently attend the UK General Dental Service. Br Dent J 2003b; 194: 329-32.
Truin GJ, Konig KG, Kalsbeek H. Trends in dental caries in The Netherlands. Adv Dent Res 1993; 7: 15-18. Twetman S, Axelsson S, Dahlgren H, et al. Caries-preventive effect of fluoride toothpaste: a systematic review. Acta Odontol Scand 2003; 61: 347-55.
Twetman S, Petersson LG, Axelsson S, et al. Caries-preventive effect of sodium fluoride mouthrinses: a systematic review of controlled clinical trials. Acta Odontol Scand 2004; 62: 223-30.
Vallis M, Ruggiero L, Greene G, et al. Stages of change for health eating in diabetes. Diabetes Care 2003; 26: 1468-74.
Van Nieuwenhuysen JP, Carvalho JC, D'Hoore W. Caries reduction in Belgian 12-year-old children related to socioeconomic status. Acta Odontol Scand 2002; 60: 123-8.
Vanobbergen J, Declerck D, Mwalili S, Martens L. The effectiveness of a 6-year oral health education programme for primary schoolchildren. Community Dent Oral Epidemiol 2004; 32: 173-82.
Vargas CM, Crall JJ, Schneider DA. Sociodemographic distribution of pediatric dental caries: NHANES III, 1988-1994. JAm Dent Assoc 1998; 129: 1229-38.
Wang NJ. Preventive dental care of children and adolescents in the 1990s: Denmark, Iceland, Norway, and Sweden. Acta Odontol Scand 1998; 56: 169-72.
Watt RG. Emerging theories into the social determinants of health: implications for oral health promotion. Community Dent Oral Epidemiol 2002; 30: 241-7.
Watt RG. From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dent Oral Epidemiol 2007; 35: 1-11.
Watt RG, Marinho VC. Does oral health promotion improve oral hygieneand gingival health? Periodontol 2000 2005; 37: 35-47.
Watt R, Sheiham A. Inequalities in oral health: a review of the evidence and recommendations for action. Br Dent J 1999; 187: 6-12.
Watt RG, McGlone P, Kay EJ. Prevention. Part 2: Dietary advice in the dental surgery. Br Dent J 2003; 195: 27-31.
Watt R, McGlone P, Evans D, et al. The prevalence and nature of recent self-reported changes in general dental practice in a sample of English general dental practitioners. Br Dent J 2004; 197: 401-5.
Yeung CA, Hitchings JL, Macfarlane TV, Threlfall AG, Tickle M, Glenny AM. Fluoridated milk for preventing dental caries [review]. Cochrane Database of Systematic Reviews 2005; Issue 3: Art. No.: CD003876. DOI: 10.1002/ 14651858.CD003876.
Figure 28.1-12
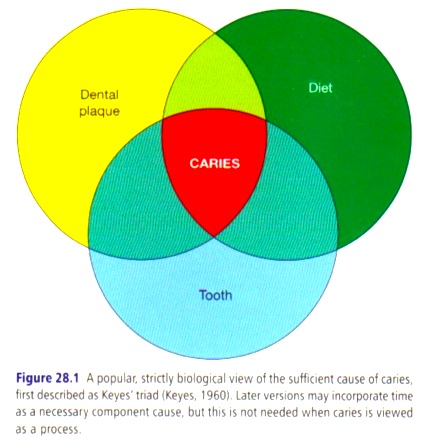 Figure 28.1 A popular, strictly biological view of the sufficient cause of caries, first described as Keyes’ triad (Keyes, 1960).
Figure 28.1 A popular, strictly biological view of the sufficient cause of caries, first described as Keyes’ triad (Keyes, 1960).
Figure 28.1 Keyesの三つの輪として知られる、有名で厳密な齲蝕の十分原因の生物学的視点 (Keyes, 1960)。
Later versions may incorporate time as a necessary component cause, but this is not needed when caries is viewed as a process.
後に、必要な構成する原因として時間の輪が加わるが、これは齲蝕を過程として見ると必要ではない。
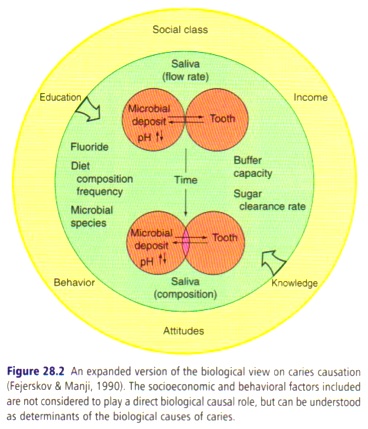 Figure 28.2 An expanded version of the biological view on caries causation (Fejerskov & Manji, 1990).
Figure 28.2 An expanded version of the biological view on caries causation (Fejerskov & Manji, 1990).
Figure 28.2 齲蝕の原因における生物学的視点の拡大 (Fejerskov & Manji, 1990)。
The socioeconomic and behavioral factors included are not considered to play a direct biological causal role, but can be understood as determinants of the biological causes of caries.
社会経済的、行動的因子は、直接生物学的因果の役割を果たしているとは考えられないが、齲蝕の生物学的原因の決定要因として理解される。
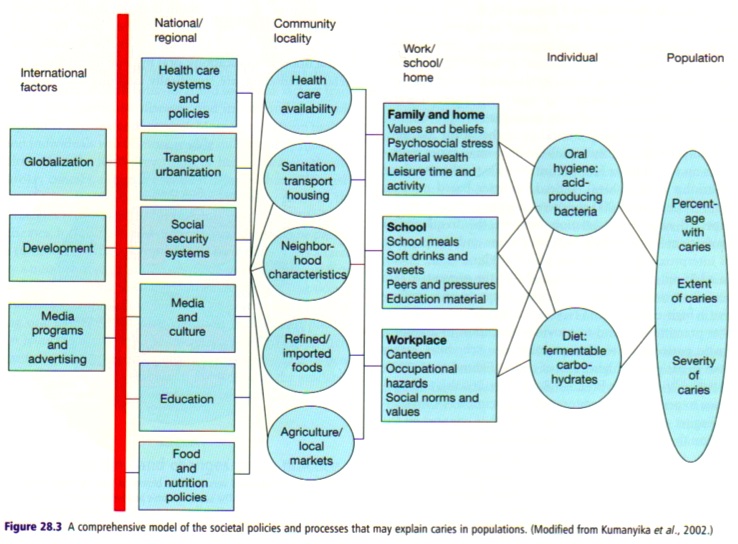 Figure 28.3 A comprehensive model of the societal policies and processes that may explain caries in populations.
Figure 28.3 A comprehensive model of the societal policies and processes that may explain caries in populations.
Figure 28.3 集団における齲蝕を説明する社会的政策と過程の包括模型。
(Modified from Kumanyika et al., 2002.)
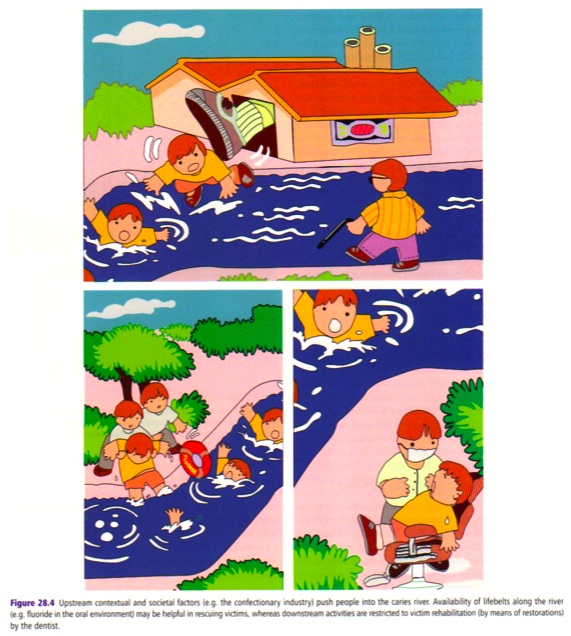 Figure 28.4 Upstream contextual and societal factors (e.g. the confectionary industry) push people into the caries river.
Figure 28.4 Upstream contextual and societal factors (e.g. the confectionary industry) push people into the caries river.
Figure 28.4 上流の(お菓子産業といった)脈絡的社会的因子が、人々を、齲蝕という名の川に後押ししている。
Availability of lifebelts along the river (e.g. fluoride in the oral environment) may be helpful in rescuing victims, whereas downstream activities are restricted to victim rehabilitation (by means of restorations) by the dentist.
川に沿って救命帯(ぶっちゃけフッ化物ね)が利用できれば、犠牲者の救出に役に立つだろうが、歯科医師による下流の活動は、犠牲者の社会復帰に制限されている。
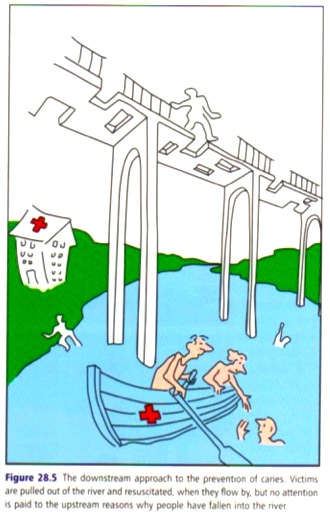 Figure 28.5 The downstream approach to the prevention of caries.
Figure 28.5 The downstream approach to the prevention of caries.
Figure 28.5 齲蝕予防の下流アプローチ。
Victims are pulled out of the river and resuscitated, when they flow by, but no attention is paid to the upstream reasons why people have fallen into the river.
流されている犠牲者は川から引き上げられ、蘇生を施される。しかし、なぜ人々が川に落下し続けるのかを上流に確認しにいくことはない。
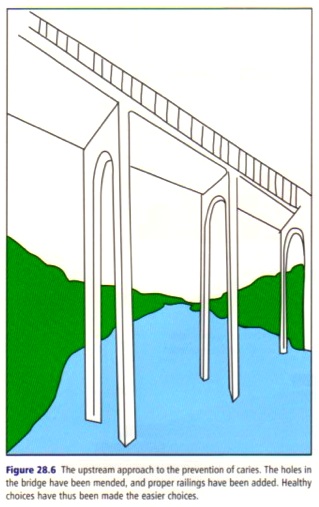 Figure 28.6 The upstream approach to the prevention of caries.
Figure 28.6 The upstream approach to the prevention of caries.
Figure 28.6 齲蝕予防の上流アプローチ。
The holes in the bridge have been mended, and proper railings have been added.
橋に開いた穴を修繕し、手すりを設ける。
Healthy choices have thus been made the easier choices.
健康的な選択をより優しい選択にする。
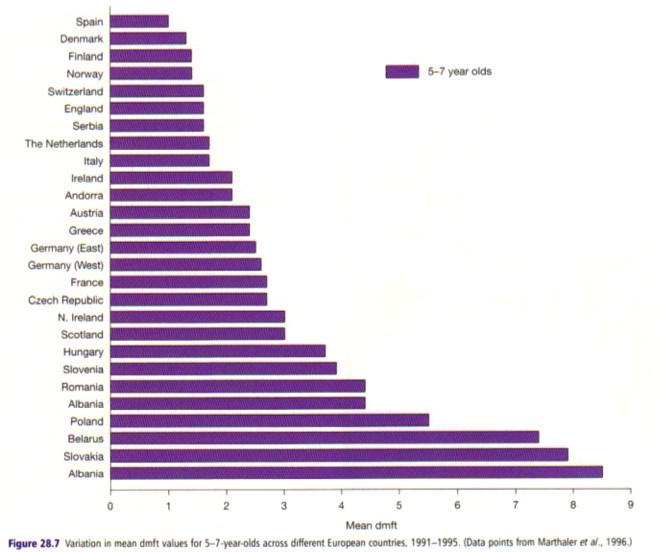 Figure 28.7 Variation in mean dmft values for 5-7-year-olds across different European countries, 1991-1995. (Data points from Marthaler et al., 1996.)
Figure 28.7 Variation in mean dmft values for 5-7-year-olds across different European countries, 1991-1995. (Data points from Marthaler et al., 1996.)
Figure 28.7 欧州の国々における5-7歳児の平均dmftの推移(1991-1995年)
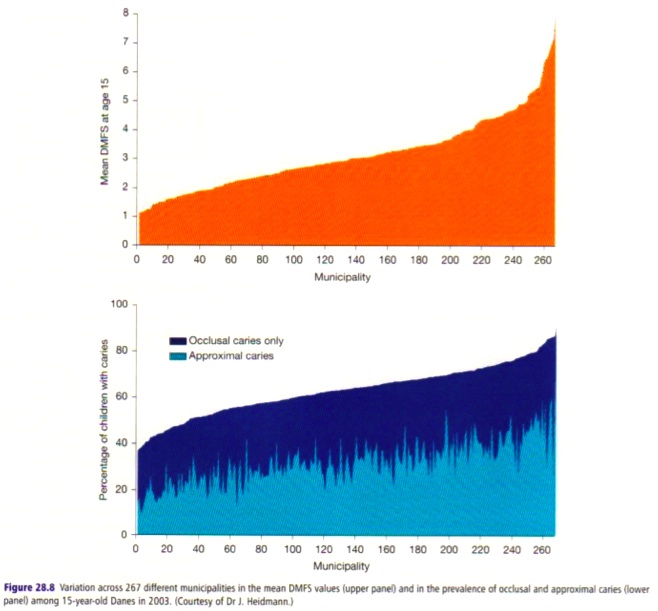 Figure 28.8 Variation across 267 different municipalities in the mean DMFS values (upper panel) and in the prevalence of occlusal and approximal caries (lower panel) among 15-year-old Danes in 2003. (Courtesy of Dr J. Heidmann.)
Figure 28.8 Variation across 267 different municipalities in the mean DMFS values (upper panel) and in the prevalence of occlusal and approximal caries (lower panel) among 15-year-old Danes in 2003. (Courtesy of Dr J. Heidmann.)
Figure 28.8 267のさまざまな地方自治体における平均DMFS指数(上)と咬合面と隣接面の齲蝕有病割合(下)の変化。2003年のデーン族の15歳児。Dr J. Heidmannの好意による。
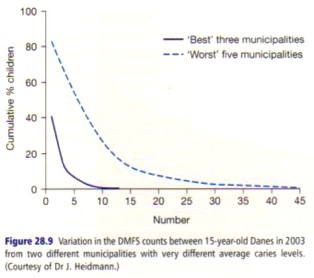 Figure 28.9 Variation in the DMFS counts between 15-year-old Danes in 2003 from two different municipalities with very different average caries levels. (Courtesy of Dr J. Heidmann.)
Figure 28.9 Variation in the DMFS counts between 15-year-old Danes in 2003 from two different municipalities with very different average caries levels. (Courtesy of Dr J. Heidmann.)
Figure 28.9 2003年のデンマークにおける15歳児におけるDMFSカウントのばらつき。平均齲蝕水準の大きく異なる、2つの地方自治体より。Dr J. Heidmannの好意による。
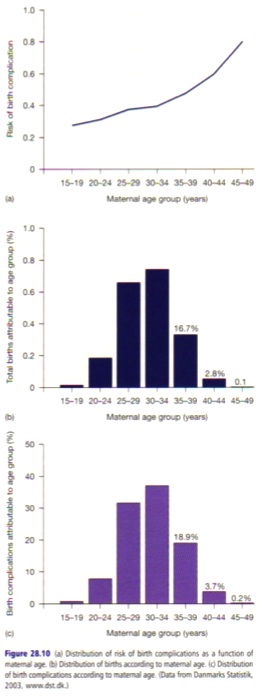 Figure 28.10
Figure 28.10
(a) Distribution of risk of birth complications as a function of maternal age.
(a) 妊娠年代ごとの出産合併症のリスク分布
(b) Distribution of births according to maternal age.
(b) 妊娠年代ごとの出産数の分布
(c) Distribution of birth complications according to maternal age.
(c) 妊娠年代ごとの出産合併症の件数の分布
(Data from Danmarks Statistik, 2003, www.dst.dk.)
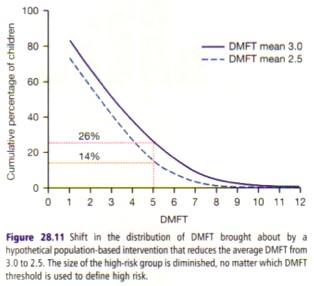 Figure 28.11 Shift in the distribution of DMFT brought about by a hypothetical population-based intervention that reduces the average DMFT from 3.0 to 2.5.
Figure 28.11 Shift in the distribution of DMFT brought about by a hypothetical population-based intervention that reduces the average DMFT from 3.0 to 2.5.
Figure 28.11 DMFT指数を3.0から2.5へ減少させる母集団介入によるDMFTカウントの分布の仮想的変化。
The size of the high-risk group is diminished, no matter which DMFT threshold is used to define high risk.
ハイリスクの基準となるDMFTカウントをどのよう変更にしても、ハイリスク集団の数は減っている。
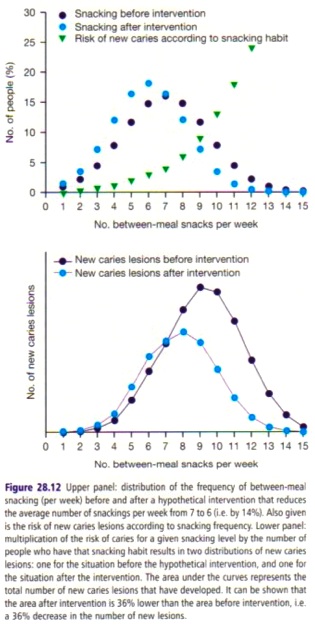 Figure 28.12 Upper panel: distribution of the frequency of between-meal snacking (per week) before and after a hypothetical intervention that reduces the average number of snackings per week from 7 to 6 (by 14%).
Figure 28.12 Upper panel: distribution of the frequency of between-meal snacking (per week) before and after a hypothetical intervention that reduces the average number of snackings per week from 7 to 6 (by 14%).
Figure 28.12 上図: 平均間食回数を週7から6に(都合14%)減らす介入前後、1週間あたりの間食の頻度の分布の予測。
Lower panel: multiplication of the risk of caries for a given snacking level by the number of people who have that snacking habit results in two distributions of new caries lesions: one for the situation before the hypothetical intervention, and one for the situation after the intervention.
下図: 間食による齲蝕リスクと間食する人数の積は、介入前後の新たなる齲蝕病巣の分布となる。
The area under the curves represents the total number of new caries lesions that have developed.
曲線より下の面積は、新たなる齲蝕病巣の総数を示している。
It can be shown that the area after intervention is 36% lower than the area before intervention, i.e. a 36% decrease in the number of new lesions.
介入後は介入前より36%小さい、つまり齲蝕病巣の数が36%減ったことが示されている。
Table 28.1-4
Table 28.1 Advantages and disadvantages of the high-risk strategy for prevention
Table 28.1 予防のためのハイリスク戦略の利点と欠点
|
Advantages
利点 | Disadvantages
欠点
|
|
Intervention is appropriate to the individual
介入は個人に適している | Prevention is medicalized
予防の医療化
|
No intervention with those not at special risk
特別なリスクのない人々には介入しない | Success palliative and temporary
成功は姑息的かつ一時的
|
Fits the ethos and organization of medical and dental care
医療と歯科医療の風潮や組織に合致 | Strategy behaviorally inadequate
行動的に不適切な戦略
|
Offers cost-effective use of resources
資源の費用効果的な利用を促す | Limited by poor prediction
予測の水準に制限される
|
Selectivity improves benefit-risk ratio
選択することで損益比を改善する | Problems of feasibility and costs
実現可能性と費用の課題
|
| Contribution to overall control of disease may be disappointingly small
疾病全体の管理への貢献は、絶望的に小さい
|
|
Table 28.2 Advantages and disadvantages of the population strategy for prevention
Table 28.2 予防のための母集団戦略の利点と欠点
|
Advantages
利点 | Disadvantages
欠点
|
|
Radical
急進的 | Acceptability may be limited
受容性に制限がある
|
Powerful
強力 | Not always feasible
実現可能性はまちまち
|
Appropriate
適切 | Costs paid now; benefits come later
投資をしても、回収までには時間がかかる
|
|
Table 28.3 The six levels in preventive dentistry
Table 28.3 予防歯科の6水準
|
Preventive level/target
予防水準/標的 | Methods
方法 | Activities/actors
活動/主体
|
Preventive level 1: Environmental change
予防水準1: 環境の変化 | Economic change
経済的変化
Social change
社会的変化
Physical change
物理的変化 | Health promotion
健康づくり
Political system/the public
政治体制/世論
|
Preventive level 2: Behavioral change
予防水準2: 行動変容 | Fluoride use
フッ化物利用
Tooth cleaning
歯磨き
Eating habits
食習慣
Use of dental services
歯科受診 | Personal
個人
|
Preventive level 3: Early diagnosis
予防水準3: 早期診断 | Screening for early disease
初期疾病のスクリーニング
Dental check-ups
歯科健診
Fluoride application
フッ化物応用
Fissure sealing and simple restorations
フィッシャーシーラントと簡単な修復 | Personal and clinical dental services
個人と臨床歯科医療
|
Preventive level 4: Preventive therapy
予防水準4: 予防治療 | Oral hygiene
口内衛生
Changing eating and drinking habits
飲食習慣の改善 | Personal and clinical dental services
個人的臨床的歯科医療
|
Preventive level 5: Rehabilitation therapy
予防水準5: 修復治療 | Restorative treatment
修復治療 | Clinical dental services
臨床歯科医療
|
Preventive level 6: Detection and prevention of impacts/disabilities/handicap
予防水準6: 影響と能力低下と社会的不利の検出と予防 | Restorative treatment of causes of sociodental impacts
社会歯科的影響の原因の修復治療 | Clinical dental services
臨床歯科医療
|
|
Table 28.4 An example of the trends for change in caries, as observed in Sweden between 1973 and 2003: the total caries burden for ages 20-70 years declined (index 100 = 1973) to 98 in 1983, 95 in 1993 and 75 in 2003.
Table 28.4 1973年から2003年にスウェーデンで観察された、齲蝕の変化の傾向の一例。20-70歳の齲蝕の全負担は1973年を100とすると、1983年は98、1993年は95、2003年は75と減少している。
|
| Age (years) | | Examination year
|
| |
|
| | 1973 | 1983 | 1993 | 2003
|
|
| 20 | Mean DFSab | 35.1 | 21.5 | 15.7 | 9.7
|
| % edentulous | - | - | - | -
|
| % of total caries burden in examination yearc | 16 | 10 | 8 | 5
|
| 30 | Mean DFSab | 48.4 | 40.7 | 23.3 | 14.0
|
| % edentulous | - | - | - | -
|
| % of total caries burden in examination yearc | 25 | 20 | 12 | 9
|
| 40 | Mean DFSab | 52.6 | 53.0 | 41.2 | 23.3
|
| % edentulous | 1.0 | - | - | -
|
| % of total caries burden in examination yearc | 18 | 28 | 21 | 16
|
| 50 | Mean DFSab | 50.5 | 53.6 | 55.2 | 34.9
|
| % edentulous | 5.0 | 3.9 | - | -
|
| % of total caries burden in examination yearc | 20 | 18 | 29 | 22
|
| 60 | Mean DFSab | 44.5 | 46.2 | 53.2 | 52.5
|
| % edentulous | 20.0 | 14.3 | 9.8 | 3
|
| % of total caries burden in examination yearc | 14 | 16 | 16 | 32
|
| 70 | Mean DFSab | 41.0 | 39.1 | 52.4 | 51.0
|
| % edentulous | 37.0 | 29.3 | 23 | 17
|
| % of total caries burden in examination yearc | 8 | 9 | 14 | 16
|
|
aIn dentate pelple.
bData for 1973, 1983 from Hugoson et al. (2000); data for 2003: personal communication.
cTotal burden for ages 20-70 years calculated by extrapolating finding to the actual Swedish population aged 20-70 years in each examination year, as reported in: http://www.scb.se/statistik/BE/BE0101/2005M05/Be0101Folkmangd1860-2004.xls
Figure 28.1-12 拡大図
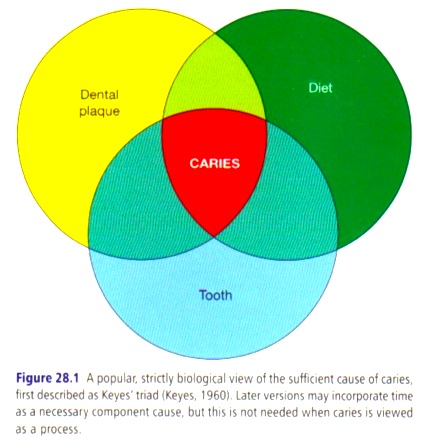
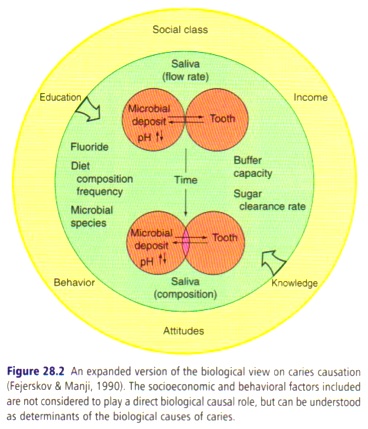
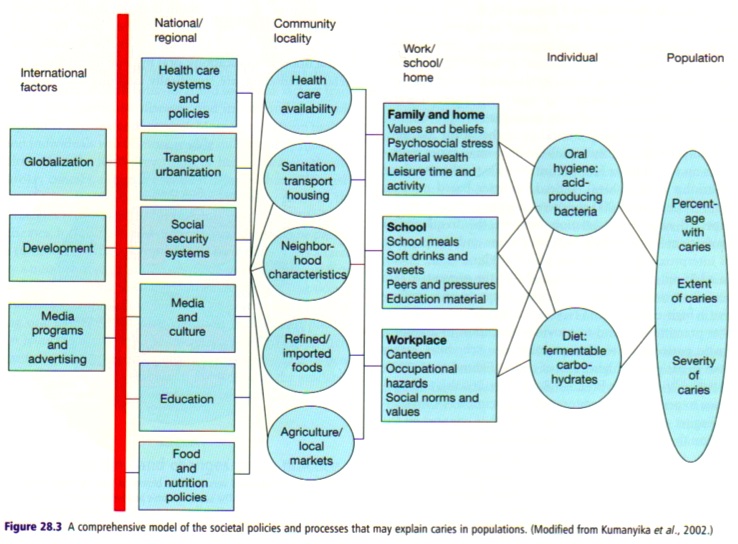
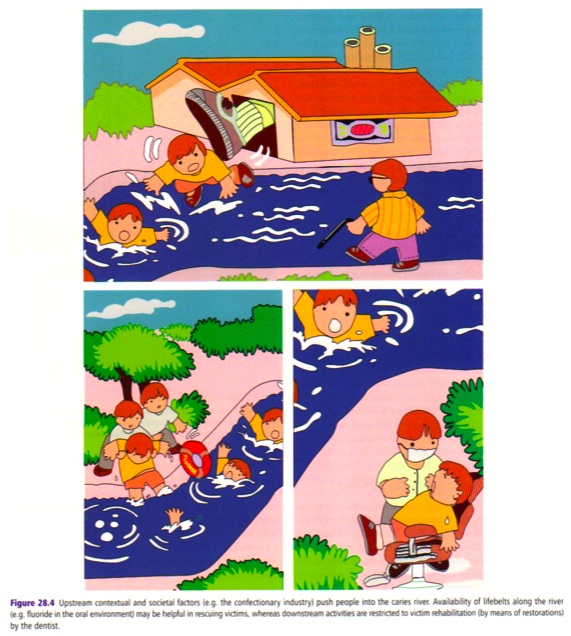
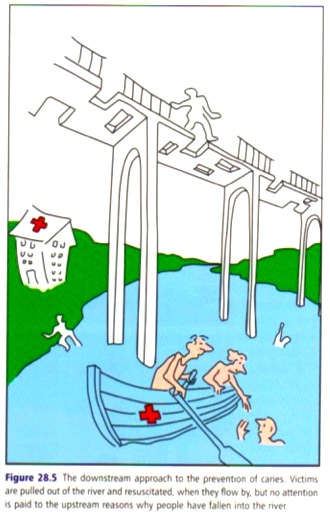
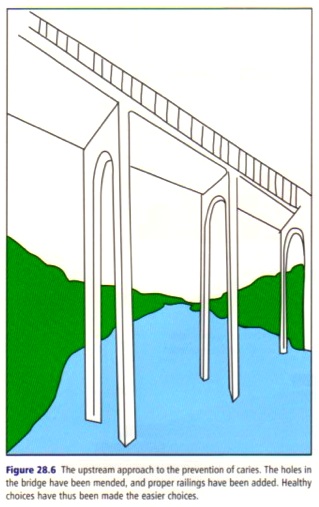
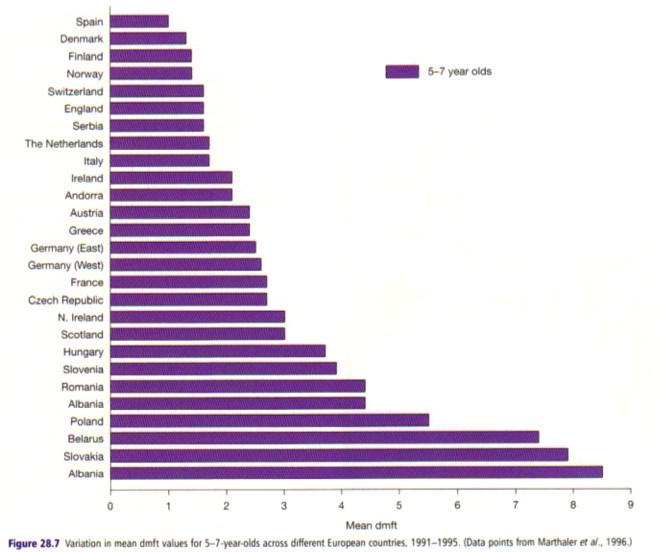
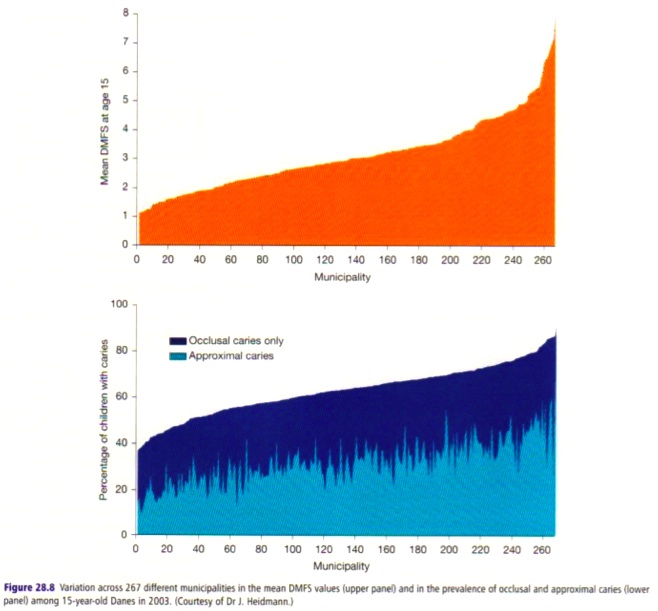
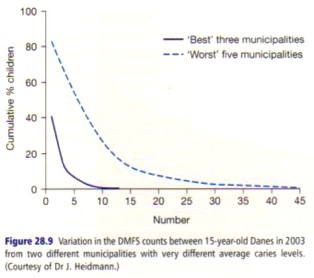
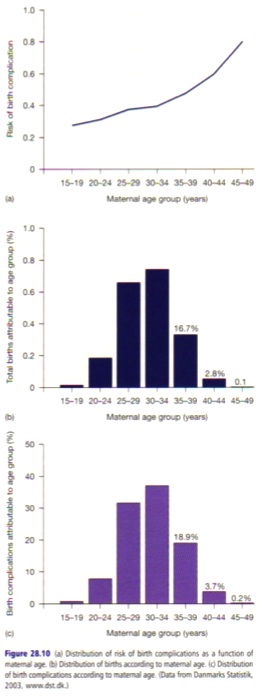
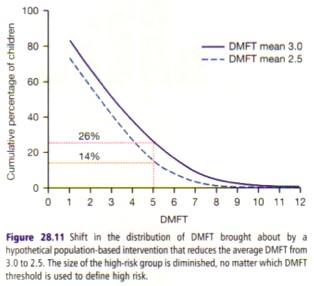
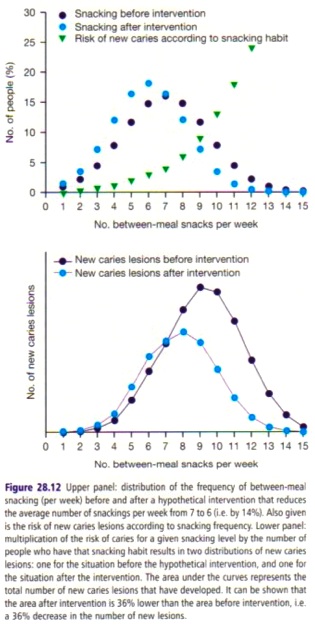
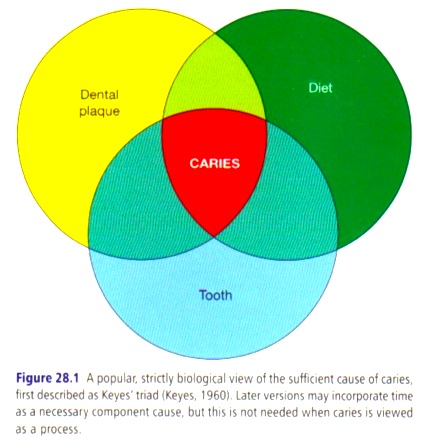 Together, these three necessary component causes form the biologically sufficient cause of caries, formerly known as Keyes’ triad (Keyes, 1960) (Fig. 28.1).
Together, these three necessary component causes form the biologically sufficient cause of caries, formerly known as Keyes’ triad (Keyes, 1960) (Fig. 28.1).